Ensuring Optimal Iodine Nutrition
Iodine Deficiency Disorders represent a significant public health threat. IFT research assessing the use of iodized salt shows the food industry is willing to use iodized salt, although numerous barriers exist around the world.
Iodine is an essential micronutrient required by the body that is found in a limited number of foods, which means that many individuals require additional sources of iodine to meet their daily requirement. Without these additional sources, a range of disorders referred to as Iodine Deficiency Disorders (IDDs) may present themselves. IDDs are the leading cause of preventable mental impairment, with more than two billion people worldwide at risk due to insufficient iodine nutrition. IDD is especially damaging during the early stages of pregnancy and in early childhood. In their most severe form, IDDs include cretinism, stillbirth, miscarriage, and increased infant mortality.
 Since 1994, the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) have recommended universal salt iodization (USI) as a safe, cost-effective, and sustainable strategy to ensure sufficient intake of iodine by all individuals. However, USI has, in practice, tended to focus only on table salt and not all salt destined for human consumption. Recent trends, particularly in industrialized countries, show that individuals are consuming the majority of their salt through processed foods, in which iodized salt is generally not used, rather than through iodized table salt. Additionally, recent initiatives to encourage reduced sodium consumption have prompted many consumers to reduce their intake of iodized table salt. While these trends in sodium consumption are more frequently observed in industrialized countries, they are expanding into many developing countries where iodine deficiency is also a concern. Thus, countries that focus on iodization of table salt alone may not achieve optimal iodine nutrition of their population.
Since 1994, the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) have recommended universal salt iodization (USI) as a safe, cost-effective, and sustainable strategy to ensure sufficient intake of iodine by all individuals. However, USI has, in practice, tended to focus only on table salt and not all salt destined for human consumption. Recent trends, particularly in industrialized countries, show that individuals are consuming the majority of their salt through processed foods, in which iodized salt is generally not used, rather than through iodized table salt. Additionally, recent initiatives to encourage reduced sodium consumption have prompted many consumers to reduce their intake of iodized table salt. While these trends in sodium consumption are more frequently observed in industrialized countries, they are expanding into many developing countries where iodine deficiency is also a concern. Thus, countries that focus on iodization of table salt alone may not achieve optimal iodine nutrition of their population.
Iodized Salt Project Parameters
The Institute of Food Technologists, under contract to the Micronutrient Initiative (MI), assessed the use of iodized salt in processed foods in 39 countries of interest to MI’s USI program (Table 1). MI is a nonprofit organization dedicated to ensuring that the world’s most vulnerable individuals, especially women and children in developing countries, get the vitamins and minerals they need to survive and thrive. The project aimed to determine if iodized salt was used in processed foods, whether or not there are policies in place to influence dietary salt reduction and how these efforts are implemented, as well as iodine nutrition knowledge among food processors in the countries of interest.
In Phase 1 of the work, IFT conducted a desk review to determine the types and level of processed food consumption in the 39 countries of interest to MI, as well as to identify suppliers of the major processed foods consumed and the use of salt as an ingredient in those products. Sixteen countries were then further evaluated in Phase 2 (Table 2). IFT reached out to food company representatives to determine their use of iodized salt in processed food products, their sources of salt, their awareness of iodine nutrition and salt as a fortification vehicle, and their interest in learning more about salt iodization.
--- PAGE BREAK ---
Processed Foods Vary by Geography
In general, processed foods consumed in many of the developing countries are not typical of what may be considered processed foods (i.e., packaged, prepared foods) in Western society. Processed foods consumed in many of the 39 countries consisted of bread, cheese, and other foods that are minimally processed compared with some of the fare available in more industrialized nations, such as convenience and snack foods, ready-to-eat meals, and so on. It is also important to note that although processed foods may be available, consumption often differs based on income and region in the country. The more affluent, and often urban, areas of countries appear more able to purchase processed foods and, therefore, more likely to have a higher consumption rate. Many of the developing nations reviewed have the highest prevalence for IDD, often due to the high levels of food insecurity. IDD is more closely linked to food insecure populations, which are also often low-income, and rural populations who lack access to food, including food that may have been prepared with iodized salt.
A pattern of processed food consumption—or lack thereof—did not present itself for the various country categories assigned to the 39 countries evaluated (see Table 1). Whether the country has a heavy (more than a million infants unprotected from IDD) or a high (between 0.5 million and 1 million unprotected infants) IDD burden or an opportunity to progress did not correlate with the consumption of processed foods in that country. IDD is present in both developed and developing countries, and countries from each of these categories may or may not have processed foods available. Some countries with the heaviest burden for IDD, such as China, may also have many processed foods available while another country with high IDD does not appear to have even minimally processed foods readily available. However, the majority of the European countries and Latin American countries identified on the list do have processed foods more readily available than some other countries identified, although not all of the foods are prepared with iodized salt.
Iodization Enforcement Challenges
Some of the developing countries have enacted legislation to combat high rates of IDD and require iodization of all salt that is to be consumed; however, they also often lack regulatory infrastructure and therefore lack effective methods to monitor and enforce salt iodization. For this reason, it appears that even when legislation and other efforts have been enacted, they are not comprehensively implemented. Whether a country has USI-related legislation varies widely, as do the specific requirements of USI-related legislation or standards when they are present, such as level of iodization, permitted iodizing substances, and enforcement. Although USI intends for all salt for human and animal consumption to be iodized (whether used in food products or not), in practice, that is not always the case. Iodized salt appears to primarily be used in food products only when required by legislation, and companies do not appear to use iodized salt in product categories that do not require it (such as beyond bread products in Australia) or for products sold in countries that do not require it.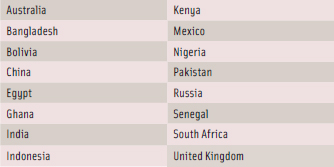
--- PAGE BREAK ---
The food manufacturers polled for Phase 2 reported potential challenges when using iodized salt in food products. These include poor stability of iodine in salt and food products, lack of enforcement of regulations, lack of resources and technical capability, potential equipment and process overhauls, and a higher cost for iodized salt (which may need to be passed on to consumers.) For example, in Pakistan, potassium iodate is not readily available, and the price varies from $2.50 to $20/kg. The average price of uniodized salt is $0.033/kg, while the average price for iodized salt doubles to $0.065/kg (Rose et. al). Consumer misconceptions about iodine’s effect on sensory/quality characteristics of food products and in the body may also be a challenge. In some countries, there are public health concerns that are deemed to be more pressing than iodine deficiency, and in food companies, competing priorities could make moving the focus to use of iodized salt in products a challenge.
In countries where the use of iodized salt in food products is not mandated, the lack of a level playing field can prevent many companies from using iodized salt since competitors may be able to sell their product for less. A lack of enforcement of regulations may create additional challenges for food producers. For example, one company may not use iodized salt in their food products but falsely claim to do so.This enables the company to either charge less for its product or increase its profit margin. Meanwhile, a competitor who uses iodized salt must either charge more or decrease its profit margin. Other challenges include trade barriers with countries that prohibit the use of iodized salt in food products or that have concerns about overconsumption of iodine. Salt suppliers also face challenges in iodizing salt in developing countries as they may not have the technical capabilities, equipment, or resources to do so.
Gauging Iodine Nutrition Awareness
Most food manufacturers report a fair level of knowledge about iodine nutrition and the use of salt as a vehicle for iodine, although individuals working for different departments in a food company will have differing levels of understanding. Most respondents noted iodine deficiency was present in their country and were aware that iodine is an essential mineral required by the thyroid for proper functioning. The main source of iodine in the diet was most often reported as iodized salt. In general, most company representatives are open to discussing iodine nutrition in more detail although it is currently discussed infrequently at most food companies. Representatives had mixed responses on whether their company would be interested in learning more about iodine nutrition although they did indicate that companies would likely be open to educational efforts to inform select company representatives about iodine nutrition.
Food companies are willing to use iodized salt in food products; however, IFT’s surveys and interviews found that the use of iodized salt in food products may need to be mandated by law as an incentive for a company to invest and to create a level playing field in the industry. Approaches to increasing voluntary use of iodized salt by food companies include outreach and education to the nutrition departments at companies, which could then recommend policy changes to top levels of management. Additionally, a consumer education campaign on the use of iodized salt in food processing to address IDD could provide incentives for companies to meet consumer demand.
Future research needs surrounding iodine use in processed foods include the need for nationwide food consumption data and additional food science research. Nationwide food consumption data is most helpful to determine processed food consumption; however, developing countries often lack the resources for such a large undertaking. Nationwide food consumption information can also reveal sources of salt intake in the diet and help to determine vehicle(s) for iodized salt delivery.
--- PAGE BREAK ---
Food science research determines the amount of iodine that should be added to a product to still meet standards after food processing and time spent on a store or consumer’s shelf. Advances in food science and technology can continue to enhance product packaging with effective barriers to protect iodine from degradation due to light, heat, and humidity, and research can further determine iodine stability throughout various processing and storage conditions. There is also concern in some countries that the use of iodized salt will negatively affect the sensory attributes of food products. Sensory studies are essential to ensure that iodization does not impact the taste or other quality attributes of a food product.
The State of Iodine Nutrition in the United States
Salt iodization is voluntary in the United States, with nearly 70% of all table salt iodized (Salt Institute, 2010). Iodine status is currently sufficient for most Americans, but iodine deficiency is re-emerging in the U.S. In fact, the National Institutes of Health’s Office of Dietary Supplements (NIH ODS) held an Iodine Workshop in May 2011 to bring together nutrition researchers, health professionals, regulators, and policymakers to shape the development of an NIH iodine initiative, and identify research needs to inform public health decisions surrounding iodine.
Agenda items included assessment and monitoring of iodine status in the U.S. and if mandatory fortification of items in the food supply is needed. In June 2011, ODS also published an iodine fact sheet for health professionals, which is available online. The Biomarkers of Nutrition for Development (BOND) Program was also recently developed by the NIH National Institute of Child Health and Human Development to support the identification of biomarkers for iodine nutrition, along with five other nutrients.
Meanwhile, movements to reduce dietary salt intake are taking place across the U.S. For example, organizations such as the New York Public Health Department have coordinated a national effort to reduce the amount of salt in packaged and restaurant foods in that state. The majority of salt intake in the U.S. comes from processed or restaurant foods (Mattes and Donnelly, 1991), and food manufacturers primarily use non-iodized salt in food products since it is not required by law. What are the implications of movements like this on iodine nutrition?
Elizabeth Pearce, an Associate Professor at the Boston University School of Medicine, acknowledges that decreased salt intake doesn’t necessarily mean poor iodine nutrition. “Decreasing salt intake can be compatible with maintaining adequate iodine nutrition, but a significant decrease in salt ingestion in the U.S. might require changes in the amount of potassium iodide added to salt in order to maintain adequate population iodine nutrition.”Kevin Sullivan, an Associate Research Professor at Emory University’s Rollins School of Public Health, concurs that “iodine status of the population must be carefully monitored should sodium consumption, especially use of household salt, be reduced substantially.”
Food manufacturers can ensure that all Americans maintain proper iodine nutrition by voluntarily using iodized salt in food products. However, Pearce notes that, “An increase in use of iodized salt by commercial food processors might necessitate a decrease in the amount of iodine added to salt in order to maintain optimal U.S. iodine nutrition.” Sullivan adds, “If changes were made concerning the use of iodized salt in the food processing industry, there would need to be a change with regards to the amount of iodine in table salt” to accommodate the increase in iodine consumption in Americans’ diets.
Iodization levels are currently based on the estimated salt consumption of 10 g/person/day. Forthcoming World Health Organization guidelines are expected to consider iodization levels based on the assumption that the consumption of salt is 5 g/person/day. Food manufacturers not ready to use iodized salt in food products should still consider how they would include iodized salt in food product formulations, processing techniques, consumer education and information, and so on, to be prepared for the use of iodized salt should it become mandatory or mandatory for select food items in the future.
Sarah D. Ohlhorst, R.D., is Director of Government Relations at the American Society for Nutrition, 9650 Rockville Pike, Bethesda, MD 20814 ([email protected]).
References
Mattes, R.D. and Donnelly, D. 1991. Relative contributions of dietary sodium sources. J. Am. College Nutr. 10(4): 383-393.
NIH. 2011. Dietary supplement fact sheet: Iodine. National Institutes of Health Office of Dietary Supplements (ODS). http://ods.od.nih.gov/factsheets/Iodine-HealthProfessional. Accessed Aug. 31, 2011.
Rose, M.A., Khan, N.A., Larik, Z., and Mohammed, F. Situational analysis of salt production and iodization in Pakistan. The Micronutrient Initiative, Pakistan; Ministry of Health, Pakistan; Integrated Marketing and Enterprise Support (IMES), Pakistan.
Salt Institute. 2010. Personal communication, June 9, 2010.
