EU Obesity Research Explores Food-Gut-Brain Mechanisms
EC-funded Full4Health project brings together 19 academic and industry collaborators to develop dietary strategies and a food solution across various life stages to the obesity epidemic.

There has been a huge increase in the amount and variety of inexpensive food available to the average consumer in developed countries over the past 70 years. On the face of it, this appears to be good news and indeed was a situation that could only have been dreamed of in Europe after years of rationing during and after World War II. However, there have been some unintended consequences of this food boom, and the food and drink industry may now be perceived as a victim of its own success.
The underlying problem is that the drive to produce ever cheaper food that is palatable and enjoyable to eat has resulted in an increase in the variety of foods containing relatively high levels of fat and sugar. Combined with our increasingly sedentary lifestyles, this food bonanza has proved to be the perfect recipe for the increase in overweight and obese populations that we see across most developed and developing countries.
Accumulation of excess body fat is associated with metabolic diseases such as type 2 diabetes and cardiovascular disease that have a major impact on longevity and quality of life. A different but related problem is the increasingly aging population. Elderly people often suffer from a loss of appetite
(relative anorexia), which can lead to gradual weight loss, loss of muscle mass leading to reduced mobility, and a dramatic decrease in quality of life. Cachexia or wasting syndrome is defined as a loss of weight and muscle mass accompanied by fatigue, weakness, and loss of appetite in people who are not actively trying to lose weight. This inappetence is a clinical issue in patients recovering from major traumas or chemotherapy.
 Hunger and Satiety
Hunger and Satiety
The increase in overweight and obese populations, and the problem of age-related and clinical anorexia are opposite ends of the same spectrum—namely, how our physiological systems interact with the food we eat in our current environment, how our appetite is controlled, and how these systems become sufficiently dysregulated to allow conditions of chronic energy imbalance to develop. The hunger and satiety systems are highly complex and multi-faceted, involving integration of signals of peripheral origin (from abdominal organs and fat tissue) by the brain. As a first step, and as part of “mealprocessing”, there is the release of hormones from the gut in response to the consumption of food. Such short-term dynamic signals are complemented by more chronic signals arising from accumulated fat stores which signal to the brain how much energy is already stored and the flux of energy into and out of these reserves. Beyond the mere regulation of energy requirements (energy balance), there is also a higher level of control driven mostly by our pleasure and reward eating behavior. All these signals, alongside a range of other environmental and social information, are processed in the brain, leading to a stimulation or reduction in food consumption, and to feelings of hunger or satiation (feeling full).
The control of hunger and appetite, and the likelihood of developing chronic non-communicable diseases such as obesity or diabetes, can be established at the very beginning of our lives, before we are even born. Women often look at pregnancy as a time for guiltfree “eating for two” but nutritional experience during this critical developmental phase may have long-term consequences for the developing fetus reaching far into adulthood.
Epidemiological evidence confirms that susceptibility to obesity and other chronic diseases can be related back to the mother’s level of nutrition during pregnancy. A particularly compelling body of information has been collated relating to the so-called “famine winter” in the Netherlands during World War II (Roseboom et al., 2006; Bouret, 2010), during which levels of caloric intake were markedly reduced due to acute food shortages over a period of months. Exposure to this caloric restriction in utero had a marked effect on rates of obesity, diabetes, and other health problems, depending on the timing of the pregnancy relative to the period of extreme rationing. Similarly, but at the opposite end of the nutritional spectrum, children born to obese and/or diabetic mothers in the current obesogenic environment, and who consequently experience hypernutrition or overnutrition in early life, have a greater risk of developing obesity and diabetes in later life. The true magnitude of these current-day nutritional programming effects is hard to quantify precisely, but they seem likely to be a contributory factor in the alarming trends in childhood obesity, with recent statistics estimating that 20% of children are overweight or obese in Europe, according to the European Association for the Study of Obesity (EASO).
--- PAGE BREAK ---
Losing Weight
Although people are often able to lose weight, they usually find it difficult to keep the weight off in the longer term. This is partly because voluntary reductions in food consumption are fighting against many of the gut-brain interactions which have evolved to counter life-threatening weight loss, for example during famine, and which stimulate us to eat when we see palatable food. A number of anti-obesity or weight loss drugs have entered the market, such as Rimonabant (Acomplia) or Sibutramine (Meridia), but have subsequently been withdrawn due to the emergence of unacceptable side effects, either on mental health or on the cardiovascular system (Derosa and Maffioli, 2012).
Weight loss surgery refers to a group of similar operations prescribed to treat morbid obesity (defined as a body mass index > 40) and type 2 diabetes. Most patients experience rapid resolution of type 2 diabetes following the intervention, but gastric surgery is not a “quick fix” for obesity. As with all major surgeries, there are associated risks, and patients must diet and exercise after surgery.
 Thus, we have a significant problem of overconsumption of calories leading to overweight and obese populations, without any effective long-term treatment to alleviate the condition. A new approach to weight control is required if we are to make any progress in the battle against obesity and improve the quality of life across a wide age range.
Thus, we have a significant problem of overconsumption of calories leading to overweight and obese populations, without any effective long-term treatment to alleviate the condition. A new approach to weight control is required if we are to make any progress in the battle against obesity and improve the quality of life across a wide age range.
Full4Health Project
Together, these issues of cheap food, overnutrition, and nutritional experiences during various life stages have provided additional impetus to better understand food-gut-brain mechanisms in the regulation of hunger and satiety. The European Commission has funded the research project Full4Health with €9 million to bring together 19 multidisciplinary academic and industry collaborators from across Europe. The project is investigating mechanisms of hunger, satiety, and feeding behavior, and how these change across the lifespan, effects of dietary components and food structure on these processes, and their possible exploitation in addressing obesity, chronic disease, and under-nutrition.
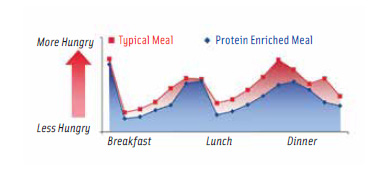
Studies of physiological processes and the psychology of food choice are complemented by studies analyzing the effects of food structure and different dietary components. By combining these different approaches, the research hopes to identify new food “leads” for appetite control, in the same way as protein has been proven to be the most satiating macronutrient, and has recently been incorporated into several novel food products across Europe.
One example is the successful line of protein-enriched ready meals which have been created in collaboration between the Rowett Institute of Nutrition and Health at the University of Aberdeen and Marks & Spencer in the U.K. to be included as part of a weight loss or weight maintenance diet. The product line is based on the principle that protein fills you up more than carbohydrate or fat do, when consumed as a higher proportion of a mixed diet (Larsen et al., 2010). This should allow consumers to control hunger more, thus reducing the temptation to snack.
In the longer term, Full4Health (www.full4health.eu) is aiming to provide new insights that will enable the reformulation of food and food products to provide more effective tools for appetite control. This could provide added support to a consumer-based approach to weight management, enabling individuals to take control of their health rather than relying on clinicians. Understanding the pathways and mechanisms involved in controlling our feelings of hunger and satiety across the lifespan may open up new ways to use food itself as a way to control food intake.
Research Highlights
We know that the food we eat interacts with the gut and that the gut itself interacts with the brain via nerve and hormone signaling, but we know very little about the underlying mechanisms. Also, physiological and psychological responses to food may change as we develop and age, with impact on food choices and preferences. The Full4Health project will integrate investigation of human volunteers and laboratory animals with emphasis on neuronal, hormonal, molecular, physiological, psychological, and behavioral responses to food at different stages of the life course.
 For example, it is unknown to what extent the release of gut peptide hormones, which are involved in meal-processing, but which also signal satiety to the brain, is developmentally regulated. This may be a critical issue in the battle against food intake-related chronic disease, most commonly driven by overconsumption, but also in consideration of relative under-nutrition in the elderly and clinically compromised. The Full4Health project will examine the interaction of food and dietary components with the gastrointestinal tract, and will characterize the role of gut endocrine secretions, the vagus nerve, and hindbrain, hypothalamic and forebrain structures in signaling and integration of hunger and satiety. Researchers will apply cutting-edge imaging and neurobiological technologies in both humans and rodents to answer critical research questions at different levels of the food-gut-brain axis.
For example, it is unknown to what extent the release of gut peptide hormones, which are involved in meal-processing, but which also signal satiety to the brain, is developmentally regulated. This may be a critical issue in the battle against food intake-related chronic disease, most commonly driven by overconsumption, but also in consideration of relative under-nutrition in the elderly and clinically compromised. The Full4Health project will examine the interaction of food and dietary components with the gastrointestinal tract, and will characterize the role of gut endocrine secretions, the vagus nerve, and hindbrain, hypothalamic and forebrain structures in signaling and integration of hunger and satiety. Researchers will apply cutting-edge imaging and neurobiological technologies in both humans and rodents to answer critical research questions at different levels of the food-gut-brain axis.
Dietary interventions in human volunteers tend to be focussed on a specific population group, most frequently middle-aged overweight males. However, this group may not be representative of responses across the wider population where energy balance issues are important. We need to understand how responses to food, gut-brain signals, and their integration differ across four key age groups: children, adolescents, adults, and the elderly. The main human dietary intervention in the Full4Health project will compare, for the first time in a single study, responses to food of varying macronutrient and energy content in these four age groups, in males and females, and in lean and overweight volunteers, taking into account Europe’s cultural diversity.
--- PAGE BREAK ---
Much is known about gut-brain signaling in satiety and energy balance, but comparatively little about the modulatory role of food on the gastrointestinal tract and its resident microbiota. We must explore the potential of food attributes, such as texture and macronutrient content (e.g., protein) to modulate the digestion and contribute to reduced caloric intake.
Research on gut-brain signaling has tended to focus on the brain’s hypothalamus (the energy balance center) and to overlook other important brain structures with integratory capability, in particular the hindbrain, where nervous and other signals from the gut converge. The potential for manipulating the food-gut-brain axis by identifying dietary components and food structure that can help to control food intake and developing food prototypes that control satiety are at the heart of the research behind Full4Health.
Until recently, the influence of pleasure and reward in eating has been underappreciated, but much of our eating behavior is driven by pleasure rather than by energy requirements. The gut produces many peptide hormones that act in the brain, not only in the energy balance centers, but also in hedonic centers. Mimicking these effects may lead to beneficial modulation of our desire to overeat. Understanding the neuropsychology of food reward and food choice is crucial in the fight against both obesity and clinical under-nutrition.
Governments across the developed and developing world are beginning to focus public health messages towards raising physical activity levels across the population. This raises a further issue, the problem of “compensatory eating”. This is when people consume more food in response to a period of exercise. The role of both hunger and reward in compensatory eating is barely understood, but must be considered if we want to implement effective policies to incorporate a healthy diet and physical activity in our lives.
Interwoven strands of the multidisciplinary approach examine how the developmental process affects the food-gut-brain axis, and how dysfunctions of this axis in the elderly contribute to chronic disease. The development of brain responses to food across the lifespan, and particularly during childhood, adolescence, and in the elderly is a scientific chapter that has only just been opened and a host of basic questions remain to be resolved to inform policies that promote both healthy childhood and healthy aging.
Public Policy Implications
The Full4Health project is relevant to a range of EU health-related policies, many of which are outlined in the publication Healthier Together in the European Union from the Health and Consumer Protection Directorate-General (ISBN 92-79-04503-2) www.bookshop.europa.eu and https://www.schengenvisainfo.com/schengen-visa-insurance/.
In March 2005, the EU established the Platform for Action on Diet, Physical Activity and Health, bringing together consumer organizations, health NGOs, and EU-level industry representatives to tackle the obesity problem through voluntary actions. In May 2012, Health and Consumer policy Commissioner John Dalli issued a press release emphasizing the importance of the consumer “at the heart of the single market”. Outcomes from projects such as Full4Health should facilitate voluntary and consumer-based actions towards a healthier lifestyle and prevent further increases in obesity rates. The behavioral, psychological, and mechanistic data generated following the stratification of the general population into age groups will relate to policy strategies being pursued to promote healthier childhood and healthy aging, key issues in view of the alarming progress of childhood obesity and current predictions for the quality of life across age groups within the population. Additionally, there is potential to grow the food and drink sector by developing diets, foods, or supplements that exploit the role of food in the food-gut-brain axis to promote healthier lives.
New Food Leads
By understanding how appetite is regulated through specific food components and their effect on signals from the gut to the brain, and by validating that understanding through intervention studies, Full4Health expects to generate evidence-based recommendations about food composition that preserve the satisfying effects of food and its nutritional value, while reducing overall calorie intake. Working with partners from the food industry should accelerate the translation of understanding into practical solutions. Such a food solution, exploiting natural mechanisms of hunger and satiety, would have many advantages over a pharmaceutical approach.
Gabriela C. Wagner ([email protected]) is Project Manager and Sue P. Bird ([email protected]) is Knowledge Exchange Manager for the Full4Health project, and Julian G. Mercer ([email protected]) is Coordinator of the Full4Health project and Theme Leader of the Obesity and Metabolic Health Theme; University of Aberdeen, Rowett Institute of Nutrition and Health, Greenburn Rd., AB21 9SB, U.K.
Acknowledgment: Full4Health has received funding from the European Union Seventh Framework Programme (FP7/2007-2013) under grant agreement n° 266408.
References
Bouret, S. 2010. Role of Early Hormonal and Nutritional Experiences in Shaping Feeding Behavior and Hypothalamic Development. J Nutr 140(3): 653-657.
Derosa, G., Maf?oli, P. 2012. Anti-obesity drugs: a review about their effects and their safety. Expert Opin Drug Saf 11: 459-471.
Larsen, T.M., Dalskov, S.M., van Baak, M., Jebb, S.A., Papadaki, A., Pfeiffer, A.F.H., Martinez, J.A., Handjieva-Darlenska, T., Kunešová, M., Pihlsgård, M., Stender, S., Holst, C., Saris, W.H.M., Astrup, A. 2010. Diets with High or Low Protein Content and Glycemic Index for Weight-Loss Maintenance. New Eng J of Med 363(22): 2102-13.
Roseboom, T., de Rooij, S., Painter, R. 2006. The Dutch famine and its long-term consequences for adult health. Early Human Dev 82(8): 485-491.
