Understanding Glycemic Impact
Some consumers are choosing foods based on their glycemic impact, but much work remains to be done on the development of low-glycemic foods.
The nutritional value of carbohydrates has become a major issue within the food industry. Consumers are no longer considering carbohydrates just as a source of calories but are now actively selecting specific types of carbohydrates for exclusion or inclusion in their diets.
 Upon digestion, carbohydrates produce glucose, which is rapidly absorbed and utilized within the body. Consumers have learned that blood sugar (glucose) levels are important because they affect their risk of developing diabetes or cardiovascular disease, weight gain, as well as mood and concentration. Numerous stories in magazines and newspapers have contributed to consumers’ understanding of blood sugar levels (e.g., Stacey, 2004). In addition, when consumers lowered the amount of processed carbohydrates in their diet, they experienced steadier energy levels, and realized that swings in blood sugar also produce swings in their perceptions of energy. As a result, consumers are now very interested in managing their blood sugar levels.
Upon digestion, carbohydrates produce glucose, which is rapidly absorbed and utilized within the body. Consumers have learned that blood sugar (glucose) levels are important because they affect their risk of developing diabetes or cardiovascular disease, weight gain, as well as mood and concentration. Numerous stories in magazines and newspapers have contributed to consumers’ understanding of blood sugar levels (e.g., Stacey, 2004). In addition, when consumers lowered the amount of processed carbohydrates in their diet, they experienced steadier energy levels, and realized that swings in blood sugar also produce swings in their perceptions of energy. As a result, consumers are now very interested in managing their blood sugar levels.
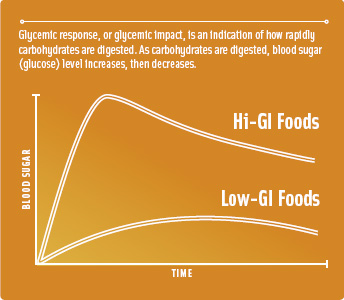
Glycemic response, or glycemic impact, is an indication of how rapidly carbohydrates are digested. The rate and peak of the increase in blood glucose from a particular food is measured by comparing it to the glycemic response of another food (typically, pure glucose). High-glycemic carbohydrates produce a fast and high increase in blood glucose level (similar to that of glucose), while low-glycemic carbohydrates produce a smaller increase relative to glucose.
Almost one in four American shoppers have decreased their consumption of high-glycemic carbohydrates within the past two years, and one in three have decreased their consumption of carbohydrates, according to the 2005 HealthFocus® Trend Report (HealthFocus, 2005) At the same time, approximately one in ten are increasing their consumption of low-glycemic carbohydrates and "better-for-you" carbohydrates. The demand for low- or reduced-glycemic foods is expected to significantly expand over the next several years, presenting significant opportunities for new product development.
There are two major challenges in formulating reduced-glycemic foods: (1) determining the analytical method for measuring the glycemic impact of the food, and (2) determining the intended marketing claim or health benefit to be communicated to consumers. These two strategic decisions will affect the selection of ingredients in food formulation. This article will briefly discuss the critical factors to be considered in these two areas.
Glycemic Index vs Response
The Glycemic Index (GI) is widely discussed around the world in the scientific and health professional communities and even some consumer circles. However, it has been criticized as a tremendously variable attribute that does not fairly represent the glycemic impact of a food or meal in the context of the entire diet. The term Glycemic Response has been also proposed and may be more appropriate for consumers, particularly regarding foods containing dietary fiber.
Glycemic Index was first defined by David Jenkins and his colleagues at the University of Toronto in 1981 (Jenkins et al., 1981), as the area under the curve for the increase in blood glucose after the ingestion of 50 g of "available" or "glycemic" carbohydrate in a food during the 2-hr postprandial period, relative to the same amount of carbohydrate from a reference food (white bread or glucose) tested in the same individual under the same conditions and using the initial blood glucose concentration as a baseline. Other reports have identified the quantity of food within the GI measurement as 50 g of carbohydrate in a food—a significantly different standard than 50 g of "glycemic" carbohydrates (FAO/WHO, 1977). The two methods of analysis produce different results, which may be significant for food formulators.
--- PAGE BREAK ---
When calculating the quantity of foods for subjects to consume in a GI test (as defined by Jenkins et al., 1981), dietary fiber is subtracted from the total carbohydrate content and additional food is consumed to deliver 50 g of "glycemic" carbohydrates. The higher the content of dietary fiber, the greater the amount of food consumed. For instance, if a bread delivered 5 g of dietary fiber/50-g serving (the carbohydrate content of bread is approximately 50%), the GI of this bread would be determined by comparing 100 g of white bread (to yield 50 g of digestible carbohydrate) with 125 g of high-fiber bread (to yield 62.5 g of carbohydrate or 50 g of available carbohydrate +12.5 g of dietary fiber).
While this comparison may be meaningful in laboratory analyses, it is meaningless to consumers, who routinely eat two slices of bread on a sandwich and would not substitute 25% more of high-fiber bread in their sandwich. Use of the GI would overestimate the impact on blood sugar of the high-fiber bread simply because it was consumed in greater quantities than the control bread within the analytical test. There is no way of identifying the comparable impact on blood sugar of equivalent quantities of these breads without re-running the test. Paper calculations (such as those utilized in the calculation of Glycemic Load, which has been defined as the weighted average GI of individual foods multiplied by the percentage of dietary energy as carbohydrate (Salmeron et al., 1997), are insufficient.
 Glycemic Response (GR) was recognized by the 2005 Dietary Guidelines Advisory Committee as the effects that carbohydrate-containing foods have on blood glucose concentration during the time course of digestion. While this definition is less standardized than the GI, it can accurately be utilized to measure the impact on blood sugar of a consistent consumer-friendly portion of food (such as that labeled as one serving on the Nutrition Facts panel). Unlike the GI, it does not penalize for the inclusion of dietary fiber, as the impact on blood sugar from identical portions of food can be compared in the determination of GR. For instance, the GR of two slices of high-fiber bread can be compared to that of two slices of white bread. However, the GR can be more difficult to compare scientifically, given the lack of standardization of measurement.
Glycemic Response (GR) was recognized by the 2005 Dietary Guidelines Advisory Committee as the effects that carbohydrate-containing foods have on blood glucose concentration during the time course of digestion. While this definition is less standardized than the GI, it can accurately be utilized to measure the impact on blood sugar of a consistent consumer-friendly portion of food (such as that labeled as one serving on the Nutrition Facts panel). Unlike the GI, it does not penalize for the inclusion of dietary fiber, as the impact on blood sugar from identical portions of food can be compared in the determination of GR. For instance, the GR of two slices of high-fiber bread can be compared to that of two slices of white bread. However, the GR can be more difficult to compare scientifically, given the lack of standardization of measurement.
The health benefits of reduced-glycemic diets have not yet been acknowledged by the American Dietetic Association, the 2005 Dietary Guidelines Advisory Committee, or other groups responsible for public health recommendations within the United States. Scientific studies have reported conflicting results regarding the health benefits of glycemic moderation, partially driven by definitions that are misused and mistakenly utilized interchangeably. In addition, confounding factors such as resistant starch further complicate the interpretation of results.
These uncertainties suggest that it is far from clear which methodology will stand the test of time. In other words, there is an inherent risk in food formulation if the glycemic methodology used is not utilized or accepted in the future. Formulating foods for a short-lived trend is more costly than formulating foods with a long life in the market.
Foods formulated for reduced glycemic impact replace glycemic carbohydrates such as sugar and flour with either (1) nondigestible carbohydrates, (2) protein, or (3) fat. As the glycemic impact is only one criterion, there is no ranking or prioritization of ingredients regarding their suitability for reducing the glycemic response. Hence, the health benefit or intended marketing claim becomes the second important criterion in ingredient selection. Blood glucose is only one factor within the body—equally important and perhaps more important is the impact of an ingredient or food on blood insulin levels. Because insulin resistance is a well-known and recognized risk factor for major diseases (Grundy et al., 2005), maintaining insulin sensitivity is critical for maintaining healthy blood sugar levels.
--- PAGE BREAK ---
Some ingredients, such as fructose and protein, do not immediately contribute to blood sugar levels, but they can increase blood insulin levels through different mechanisms. For instance, one study (Hertzler and Kim, 2003) found that low and moderate glycemic nutrition bars had lower glycemic responses but significantly higher insulin responses than expected and actually had insulin impact similar to that of a high-carbohydrate, high-glycemic nutrition bar. The authors attributed the results to the higher protein content of these bars, as several studies have shown dietary protein and/or specific amino acids to be insulinogenic.
A recent review of GI methodology found that proteins can cause greater insulin secretion when combined with carbohydrates, further confusing the issue and suggesting that the final foods must be tested (Brouns et al., 2005). Thus, a food’s glycemic impact alone cannot be used to estimate benefits delivered by low-insulinemic foods and foods that help maintain insulin sensitivity.
Reducing Glycemic Impact
Sugar substitutes and low-glycemic sweeteners have been used to replace sugar to reduce the glycemic impact of foods. However, the impact on insulin is less clear. While glucose is used as the standard with a GI of 100, sucrose (table sugar) has a GI of 65. Sucrose is a disaccharide of glucose and fructose. Upon cleavage of the disaccharide bond, the glucose is rapidly absorbed and rapidly raises blood glucose levels, while the fructose is absorbed and metabolized in the liver at a slower rate. However, while fructose may be low glycemic, it has been shown to promote insulin resistance (Basciano et al., 2005). Thus, any health benefits of low-glycemic foods which rely on reduced insulin levels would not be delivered by fructose-containing sweeteners. In general, reducing the sugar content of foods by nondigestible sweeteners would reduce the glycemic and insulin response of that food if the bulk of the sugar were not replaced by other digestible carbohydrates.
Whole grains may or may not reduce the glycemic impact of foods. If the whole-grain food retains the fiber and the natural resistant starch content of the grain, it will likely have a lower glycemic impact. However, if the whole-grain food is processed and lacks dietary fiber and its inherent resistant starch, it will have a higher glycemic impact and offer minimal or modest reductions in glycemic response.
For instance, whole-grain wheat contains approximately 14% resistant starch, but processing it into flour reduces its resistant starch content to 2% (Bednar et al., 2002). According to the 2002 International Table of GI and Glycemic Load Values (Foster-Powell et al., 2002), coarse-kernel wheat breads, coarse-kernel rye breads, and coarse-kernel barley breads had a reduced GI, but whole-wheat-flour breads were essentially identical in their GI to white bread. In general, the less-processed whole grains deliver a lower glycemic impact but are more difficult to work with in processed foods and can significantly change the texture of food.
Resistant starch has been used to replace flour, but it may or may not reduce the glycemic response of foods. One published study indicated that chemically modified resistant starch (RS4 type) increased the glycemic response of foods and had no impact on the insulin response (Zhou and Kaplan, 1997). In contrast, natural resistant starch from high-amylose corn has been shown to reduce the glycemic response and the insulin response of foods in published studies when it is used as a flour substitute (Jones et al., 2005).
In addition, recent studies have shown that natural resistant starch increases insulin sensitivity in healthy humans (Robertson et al., 2005). The 33% increase in insulin sensitivity was not based on its reduced glycemic or insulin impact, but rather on its fermentation within the large intestine and its production of short-chain fatty acids. This combination of physiological attributes makes it a valuable ingredient in formulating low-glycemic foods.
--- PAGE BREAK ---
Natural (RS2 type) resistant starches also offer functional benefits. These starches, which maintain their natural granular structure, test as insoluble dietary fiber, have a low water-holding capacity, and easily replace flour in food formulations (and in home baking). In contrast to other fibers that hold significant amounts of water, resistant starches do not affect dough handling or mixing characteristics or significantly alter baking time.
Much work remains to be done on the development of low-glycemic foods, including the confirmation of particular benefits and understanding of the mechanisms for the delivery of those benefits. The careful selection of targets, ingredients, and formulation strategies will go a long way toward achieving long-term success.
Consumer Study Addresses Reduced-Glycemic Foods
At a conference on resistant starch in September 2005, sponsored by Oldways Preservation Trust and Natural® Hi-maize, The 5-in-1 Fiber, Linda Gilbert, President of HealthFocus International®, reported on the previously unpublished results of the 2005 HealthFocus Trend Survey. This study, sponsored by National Starch, manufacturer of Hi-maize, focused on identifying consumer perspectives and preferences regarding dietary fiber and its benefits.
"Fiber is not a benefit for consumers. It is support for a benefit promise" said Linda Gilbert, President of HealthFocus. "Although consumers don’t understand Glycemic Index, they understand its impact on their lives from stress and tiredness for themselves, to crankiness and irritability for their children."
According to the proprietary study, 69% of shoppers want to learn more about fibers that reduce hunger and help control your appetite, 65% about carbohydrates that help keep your energy in balance, 64% about foods that help with digestion, and 60% about foods with a low impact on blood sugar levels. Also, 64% of shoppers with children in their household want to learn more about carbohydrates that will give your children more manageable energy.
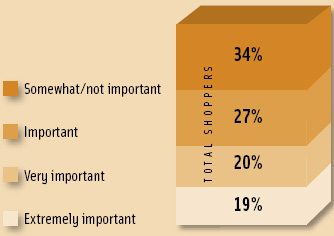 Within the American population, there is a high awareness of some of the benefits of blood sugar management—53% have heard a lot or some about blood sugar and energy; 51% also strongly believe or believe that eating foods with a low impact on blood sugar helps to maintain energy levels in the hours following a meal; and 66% feel that helps to maintain healthy blood sugar levels is an important label claim on foods (19% extremely important). This is surprising, as this label statement has not yet occurred on food labels in the United States. It indicates a strong, unmet opportunity for new product development.
Within the American population, there is a high awareness of some of the benefits of blood sugar management—53% have heard a lot or some about blood sugar and energy; 51% also strongly believe or believe that eating foods with a low impact on blood sugar helps to maintain energy levels in the hours following a meal; and 66% feel that helps to maintain healthy blood sugar levels is an important label claim on foods (19% extremely important). This is surprising, as this label statement has not yet occurred on food labels in the United States. It indicates a strong, unmet opportunity for new product development.
Glycemic-management claims can broaden the appeal of high-fiber foods. Traditionally, interest in dietary fiber grows as people age. The challenge is in marketing the benefits to younger populations. For instance, 38% of American grocery shoppers claim that they always or usually maintain a high-fiber diet, but only 27% of shoppers in their 30s do. Similarly, 38% of all shoppers state that high fiber is an extremely or very important claim on food labels, compared to only 30% of shoppers age 18–29. In contrast, American grocery shoppers age 30–39 are most likely to strongly believe or believe that eating foods that have a low impact on blood sugar levels help to balance your energy in the hours following a meal (57% vs 44% for those over age 65). Furthermore, shoppers age 30–49 are also most likely to strongly believe or believe that eating foods that release energy slowly can help you lose weight. At the same time, 51% of shoppers age 30–39 stated that Glycemic Index had no influence on their choice while shopping. Thus, focusing on the energy and weight benefits of glycemic moderation increases the appeal of reduced-glycemic foods in younger populations, more than focusing on the nutritional content of fiber or the technical description of Glycemic Index.
Consumer recognition of the technical term "Glycemic Index" or "Glycemic" is relatively low—28% of shoppers have heard a lot or some about low-glycemic foods, compared to 53% who have heard a lot or some about blood sugar and energy). Currently, approximately 1 out of 4 primary grocery shoppers within the U.S. report that "Glycemic Index" is a moderate or strong influence on their choice of foods, and 7% of shoppers are increasing their use of low-glycemic carbohydrates.
All indications suggest that glycemic management will be a major driver for consumers with regard to carbohydrate consumption. Based on this research, the many and varied benefits of glycemic control will be more appealing to consumers than the nutritional content alone. Thus, the selection of food and/or ingredients that contribute to the health benefits becomes just as important as, if not more important than, the glycemic response number or dietary fiber content alone.
by Rhonda Witwer is Business Development Manager of Nutrition, National Starch Food Innovation, 10 Finderne Ave., Bridgewater, NJ 08807-3355 ([email protected]).
References
Basciano, H., Federico, L., and Adeli, K. 2005. Fructose, insulin resistance, and metabolic dyslipidemia. Nutr. Metabolism 2: 5. www.nutritionandmetabolism.com/content/2/1/5.
Bednar, G.E., Patil, A.R., Murray, S.M., Grieshop, C.M., Merchen, N.R., and Fahey, G.C. Jr. 2002. Starch and fiber fractions in selected food and feed ingredients affect their small intestinal digestibility and fermentability and their large bowel fermentability in vitro in a canine model. J. Nutr. 56: 500-505. www.nutrition.org/cgi/content/abstract/131/2/276.
Brouns, F., Bjorck, I., Frayn, K.N., Gibbs, A.L., Lang, V., Slama, G., and Wolever, T.M.S. 2005. Glycaemic index methodology. Nutr. Res. Rev. 18(1): 145-171.
FAO/WHO. 1997. Carbohydrates in human nutrition, a Joint FAO/WHO Expert consultation, Rome, April 14–18. FAO Food and Nutrition Paper 66, p. 25. Food and Nutrition Org./World Health Org., Rome. www.fao.org/docrep/w8079e/w8079e00.htm.
Foster-Powell, K., Holt, S.H.A., and Brand-Miller, J.C. 2002. International table of glycemic index and glycemic load values: 2002." Am. J. Clin. Nutr. 76: 5-56. www.ajcn.org/cgi/content/full/76/1/5.
Grundy, S.M,, Cleeman, J.I., Daniels, S.R., Donato, K.A., Eckel, R.H., Franklin, B.A., Gordon, D.J., Krauss, R.M., Savage, P.J., Smith, S.C., Spertus, J.A., and Costa, F. 2005 Diagnosis and management of the metabolic syndrome. An American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. http://circ.ahajournals.org/cgi/reprint/circulationaha.105.169405v1
HealthFocus. 2005. The 2005 HealthFocus® Trend Report: The national study of public attitudes and actions toward shopping and eating. HealthFocus International®, St. Petersburg, Fla.
Hertzler, S.R. and Kim, Y. 2003. Glycemic and insulinemic responses to energy bars of differing macronutrient composition in healthy adults. Med. Sci. Monitor 9(2): CR84-90. www.medscimonit.com/pub/vol_9/no_2/3230.pdf.
Jenkins, D.J., Wolever, T.M., Taylor, R.H., et al. 1981. Glycemic index of foods: A physiological basis for carbohydrate exchange. Am. J. Clin. Nutr. 34: 362-366.
Jones, J.M., Witwer, R., and Birkett, A. 2005. High amylose corn resistant starch monograph. Sept., p. 7. National Starch Food Innovation, Bridgewater, N.J.
Robertson, M.D., Bickerton, A.S., Dennis, A.L., Vidal, H., and Frayn, K.N. 2005. Insulin-sensitizing effects of dietary resistant starch and effects on skeletal muscle and adipose tissue metabolism. Am. J. Clin. Nutr. 82: 559-567. www.ajcn.org/cgi/content/abstract/82/3/559.
Salmeron, J., Manson, J.E., Stampfer, M.J., Colditz, G.A., Wing, A.L., and Willett, W.C. 1997. Dietary fiber, glycemic load, and risk of non-insulin-dependent diabetes mellitus in women. J. Am. Med. Assn. 277: 472-477.
Stacey, M. 2004. Let them eat cake. O the Oprah Magazine, July, pp. 107-111.
Zhou, X. and Kaplan, M.L. 1997. Soluble amylose cornstarch is more digestible than soluble amylopectin potato starch in rats. J. Nutr. 127: 1349-1356. www.nutrition.org/cgi/content/full/127/7/1349.
