Circulating Heart-Smart News
NUTRACEUTICALS & FUNCTIONAL FOODS
“The way to a man’s heart is through his stomach,” the old saying goes. And with 61 million Americans afflicted by one or more forms of cardiovascular disease (CVD), it may very well be that to keep people’s hearts healthy, Americans will have to pay more attention to what they are eating.
According to statistics from the American Heart Association (AHA), CVD claimed 958,775 lives in 1999. This is equivalent to 40.9% of all deaths or one out of every 2.5 deaths. In addition, almost 150,000 Americans killed by CVD are under age 65.
Forms of CVD include high blood pressure and coronary heart disease (CHD), the single leading cause of death in America today. CHD is caused by atherosclerosis, the narrowing of the coronary arteries due to fatty buildup of plaque. Risk factors include high total cholesterol levels and high levels of low-density-lipoprotein (LDL) cholesterol. High CHD rates occur among people with high blood cholesterol levels of 240 mg/dL or above and LDL-cholesterol levels of 160 mg/dL or above.
There is no doubt that dietary factors influence the risk of CVD, both favorably and unfavorably. Diets high in saturated fat and sodium increase the risk, while diets high in fiber and antioxidants can help prevent CVD. Although moderation of foods is important, consumers still look for holy-grail ingredients that they believe will help their hearts. This may explain why the heart supplement market is estimated at $750 billion per year.
Heart-Healthy Nutraceuticals
Research shows that some nutraceuticals help prevent the risk of CVD:
• Soy Protein and Isoflavones. According to a 2001 United Soybean Board survey, on an unaided basis, 39% of consumers said they were aware of specific health benefits of soy in the diet. Of those, 42% were aware that soy may lower cholesterol and reduce the risk of heart disease, compared to 24% in 1999.
This increase in awareness is largely due to the Food and Drug Administration’s October 1999 authorized health claim about the role of soy protein in reducing the risk of CHD. FDA concluded that foods containing soy protein included in a diet low in saturated fat and cholesterol may reduce the risk of CHD by lowering blood cholesterol levels.
Scientific studies show that 25 g of soy protein daily in the diet is needed to show a significant cholesterol-lowering effect. To qualify for this health claim, a food must contain at least 6.25 g of soy protein per serving.
Foods that may be eligible for the health claim include soy beverages, tofu, tempeh, soy-based meat alternatives, and possibly some baked goods. Tofu satay with soy butter sauce (Fig. 1) is one example of a product that could carry the claim. Foods that carry the claim must also meet the requirements for lowfat, low saturated fat, and low cholesterol content. Foods made with the whole soybean may also qualify for the health claim if they contain no fat in addition to that present in the whole soybean.
--- PAGE BREAK ---
Research is also focusing on soy isoflavones and their ability to lower plasma cholesterol. The mechanism for this capability is still not fully understood. Since soy isoflavones contain phenolic groups, they may possess antioxidant functions to protect against oxidation of cholesterol and oxidative damage to blood vessel cells.
Scientists at Louisiana State University’s Agricultural Center recently investigated antioxidant activities of the soy isoflavones genistein and daidzein in preventing cholesterol oxidation, using a chemical model system. The two isoflavones demonstrated significant antioxidant activity in the inhibition of cholesterol oxidation. Results indicated that the antioxidant functions of daidzein and genistein may contribute to the potential hypocholesterolemic and anti-cancer properties of soybean.
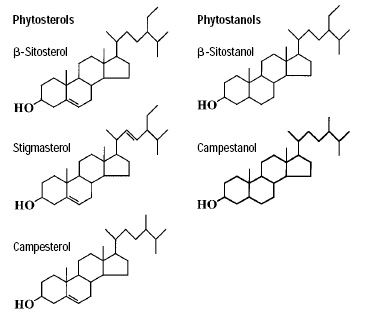 • Plant Sterols and Stanols. AHA currently recommends that plant sterol-containing foods should be reserved for adults who require lowering of total and LDL cholesterol levels because of hypercholesterolemia or the need for secondary prevention after an atherosclerotic event. Scientific studies show that 1.3 g of plant sterol esters or 3.4 g of plant stanol esters per day in the diet is needed to show a significant cholesterol-lowering effect (Fig. 2).
• Plant Sterols and Stanols. AHA currently recommends that plant sterol-containing foods should be reserved for adults who require lowering of total and LDL cholesterol levels because of hypercholesterolemia or the need for secondary prevention after an atherosclerotic event. Scientific studies show that 1.3 g of plant sterol esters or 3.4 g of plant stanol esters per day in the diet is needed to show a significant cholesterol-lowering effect (Fig. 2).
Plant sterols are present in small quantities in many fruits, vegetables, nuts, seeds, cereals, legumes, and other plant sources. Plant stanols occur naturally in even smaller quantities from some of the same sources. In September 2000, FDA authorized the use of health claims about the role of plant sterol or plant stanol esters in reducing the CHD risk for foods containing these substances.
Foods that may qualify for the health claim based on plant sterol ester content include spreads and salad dressings. Among the foods that may qualify for claims based on plant stanol ester content are spreads, salad dressings, snack bars, and dietary supplements in softgel form.
To qualify for the claim, a food must contain at least 0.65 g of plant sterol esters or 1.7 g of plant stanol esters per serving. The claim must specify that the daily dietary intake of plant sterol esters or plant stanol esters should be consumed in two servings eaten at different times of the day with other foods.
Foods that carry the health claim must also meet the requirements for low saturated fat and low cholesterol, and must also contain no more than 13 g of total fat per serving and per 50 g. However, spreads and salad dressings are not required to meet the limit for total fat per 50 g if the label of the food bears a disclosure statement referring consumers to the Nutrition Facts panel of the label for information about fat content.
In addition, except for salad dressing and dietary supplements, the food must contain at least 10% of the Reference Daily Intake (RDI) or Daily Reference Value (DRV) for vitamin A, vitamin C, iron, calcium, protein, or fiber. FDA also requires, consistent with other health claims to reduce the risk of CHD, that the claim state that plant sterol and plant stanol esters should be consumed as part of a diet low in saturated fat and cholesterol.
--- PAGE BREAK ---
• Dietary Fiber. AHA recommends a total dietary fiber intake of 25–30 g/day from foods, not supplements, to ensure nutrient adequacy and maximize the cholesterol-lowering impact of a fat-modified diet. Current dietary fiber intakes among adults in the United States, however, average about 15 g/day, or about half the recommended amount.
Research provides evidence that dietary fiber acts in the gastrointestinal tract to reduce blood cholesterol by decreasing absorption of cholesterol or fatty acids and of biliary cholesterol or bile acids. Fiber may also cause altered serum concentration of hormones or short-chain fatty acids that affect lipid metabolism. Beta-glucan, the water-soluble fiber prevalent in oats and barley, has been shown in animal models to be the active agent causing the altered cholesterol metabolism.
In February 2002, General Mills, Minneapolis, Minn., began conveying the importance of lowering cholesterol on its Honey Nut Cheerios® boxes (Fig. 3, on page 114). The company challenged Americans to “Bee Happy, Bee Healthy” by taking simple steps to lower their cholesterol. The label emphasizes the product’s soluble fiber content, stating, “May Lower Cholesterol as part of a lowfat diet with the soluble fiber in Honey Nut Cheerios. As part of a lowfat diet, 3 grams of soluble fiber daily can help reduce blood cholesterol. Honey Nut Cheerios, with its natural, sweet taste of honey, now provides .75 grams of soluble fiber in a 1-cup serving.”
• Vitamins B-6, B-12, and Folic Acid. David Kritchevsky, scientist at the Wistar Institute of Anatomy and Biology, Philadelphia, Pa., said that these vitamins will lower levels of artery-toxic homocysteine. Homocysteine has been shown to have pro-oxidant properties, to up-regulate thrombotic function, and to attenuate nitric oxide release. Thus, homocysteine is a possible marker for the development of vascular disease.
Studies at Brown University focused on how B-6, B-12, and folic acid deficiencies can elevate homocysteine levels and lead to arteriosclerosis. According to the research, when homocysteine levels rise, they begin to damage the cells and tissues of healthy arteries and stimulate growth of arteriosclerotic plaques, which can lead to heart disease.
The normal metabolism of homocysteine requires an adequate supply of folate, vitamin B-6, vitamin B-12, and riboflavin. Lower folate concentrations have been associated with increased coronary disease risk, and a significant association between lower folate levels and fatal coronary artery disease has also been reported.
• Omega-3 Fatty Acids. Consumption of one fatty fish meal per day (or alternatively, a fish oil supplement) could result in an omega-3 fatty acid intake of 900 mg/day, an amount shown to beneficially affect CHD mortality rates in patients with coronary disease.
Long-chain omega-3 fatty acids from fish oil decrease triglyceride levels, favorably affect platelet function, and decrease blood pressure slightly in hypertensive individuals. Controlled clinical trials have demonstrated beneficial effects of diets high in omega-3 fatty acids on CHD.
--- PAGE BREAK ---
The April 2002 issue of AHA’s journal Circulation reported that daily supplements of a fatty acid found in fish oil halves the risk of sudden death in heart attack survivors. Previous research had found that eating oily fish such as tuna and salmon can reduce the risk of sudden cardiac death caused by a particular type of irregular heartbeat. This study suggested that fish-oil supplements, rather than dietary fish oil, could be a therapy without side effects for heart patients.
• Arginine. Arginine is good for arterial health, said Kritchevsky. The average American consumes 4–5 g of L-arginine per day, and red meat is the most frequently consumed source. Other dietary sources include walnuts, peanuts, soybeans, legumes, and fish protein. Clinical studies of L-arginine, a nitric oxide precursor, have shown significant effects when intake is increased three- to fourfold via supplements.
For example, work cited in Journal of Clinical Investigations in 1996 showed that 4 weeks of oral L-arginine supplements (21 g/day) produced a two-fold increase in flow-mediated dilation (FMD) of the brachial artery in hypercholesterolemic patients. A large change in diameter during FMD indicates healthy vessels. The vascular benefits may only be observed in patients with impaired nitric oxide status, such as hypercholesterolemic patients and individuals with established peripheral arterial disease.
Other Noteworthy Nutraceuticals
Ongoing research continues to explore heart-health benefits of the following potential nutraceuticals:
• Conjugated Linoleic Acid and Avocado Oil. Kritchevsky’s lab at the Wistar Institute currently works with conjugated linoleic acid (CLA) and avocado oil and the role of fat metabolism in diseases such as cancer and heart disease. His is the first laboratory to investigate the effects of CLA in experimental atherosclerosis in rabbits. “We have found in two studies that CLA fed as 1.0% of the diet significantly inhibits atherogenesis. CLA also exerts a protective effect at dosages as low as 0.1% of the diet. This level of protection against atherosclerosis has been observed using other dietary or pharmacologic agents,” he explained.
Review of the literature shows that returning rabbits with pre-established lesions to a cholesterol-free diet or diet plus cholesterol-lowering drugs generally leads to increased severity of lesions by 30–40%, Kritchevsky added. “We have demonstrated that inclusion of 1% CLA in a cholesterol-free diet fed to rabbits with pre-established lesions reduces the severity of those lesions by 32%. This is, to our knowledge, the first regression of this magnitude.”
“Avocado oil is similar to olive oil in that it raises high-density lipoprotein (HDL) levels in rabbits; however there is no effect on LDL,” Kritchevsky stated. Avocado oil is rich in oleic acid. When fed to cholesterol-fed rabbits, it significantly reduces severity of aortic lesions (compared to coconut oil) and raises the level of plasma HDL.
• Vitamin D. Research presented at an AHA Asia Pacific Scientific Forum in April 2002 revealed that women over age 65 who took vitamin D had nearly one-third less risk of dying from heart disease as women who did not take the supplements. “Low blood levels of certain forms of vitamin D have been associated with increased risk of heart attacks, but to my knowledge no one has studied whether vitamin D supplements affect the risk of heart disease events,” said Paul D. Varosy, M.D., a fellow in cardiology and medicine at the University of California at San Francisco and the San Francisco VA Medical Center.
--- PAGE BREAK ---
The researchers studied 9,704 women ages 65 and older enrolled in the Study of Osteoporotic Fractures. The subjects included 4,272 women who reported current use of vitamin D supplements. During an average followup period of nearly 11 years, 420 of the women died of CHD. Women who used vitamin D supplements had 31% less risk of heart disease death than those who did not take the supplements. The use of calcium supplements did not affect those results. Researchers controlled for possible factors that could alter results, such as heart disease risk factors, calcium supplement use, self-reported health status, education, and behaviors such as exercise and smoking.
“In short, the benefits we observed seemed due to vitamin D and not due to calcium,” Varosy said. Vitamin D, which is both a hormone and a vitamin, is one of the most important regulators of calcium absorption in the body. Atherosclerois is often associated with calcification, the buildup of the mineral calcium in the arteries.
“A lot of evidence suggests that calcification in the arteries is very similar to the calcification process that occurs in bone,” he said. Earlier studies had suggested that low blood levels of vitamin D might play a role in the calcification that may contribute to heart disease. “In fact,” he added, “women with osteoporosis tend to have more calcium in the walls of their arteries than women with normal bones.”
• Garlic. With consumer interest in botanicals, garlic has also stepped into the limelight for its medicinal properties. Several studies have indicated garlic to be effective in lowering blood cholesterol, reducing the level of other fats in the blood, reducing the tendency of the blood to clot, and preventing coronary artery disease. Research indicates that the most active compounds in garlic contain sulfur, which is primarily responsible for its potency and for effectively reducing blood cholesterol levels by slowing the body’s own manufacture of cholesterol and helping the body eliminate cholesterol by transporting fats from the tissues to the bloodstream. According to ActiveHealth.com, clinical research shows that a dose of only one to two cloves of garlic per day will lower cholesterol by about 15%.
The May 1999 issue of Atherosclerosis published the results of a “pharmaceutical-quality” clinical trial using garlic. Involving 280 people, the four-year, double-blind, randomized, placebo-controlled study documented that using Kwai Garlic daily prevented the buildup of plaque in arteries. “The results of the study are remarkable, because over four years there was a significant reduction in the progression of plaque build-up, and even a reduction in plaque size in some cases,” said Haris Boudoulas, professor of medicine and pharmacy at Ohio State University’s Division of Cardiology.
• Coenzyme Q10. “CoQ10 is an essential component of the energy-producing systems of the body’s cells,” said Phillip Harvey, Chief Science Officer at the National Nutritional Foods Association, Newport Beach, Calif. “It has been studied extensively throughout the world and has numerous applications, including antioxidant function, and therapeutic approaches to numerous diseases affecting the cardiovascular system, diabetes, and musculoskeletal disorders.”
CoQ10 is a lipid-soluble benzoquinone occurring naturally in the body and in smaller amounts in most foods, especially meats and seafood. Scientific data have shown that CoQ10, when used as a dietary supplement, has strong clinical applications in congestive heart failure, cardiac arrhythmias, angina, and hypertension. Sales of this specialty supplement reached $170 million in 2000, according to Nutrition Business Journal.
--- PAGE BREAK ---
• Chocolate. And for research that sounds sweet to many people’s ears, eating chocolate can help prevent LDL cholesterol and hardening of arteries. U.S. researchers believe that by following a diet high in flavonoid-rich cocoa powder and dark chocolate, consumers can witness a positive effect on their LDL levels, as opposed to other diets that limit or exclude flavonoid sources such as tea, coffee, wine, and onions. The study was published in the November 2001 issue of the American Journal of Clinical Nutrition.
Scientists at Penn State University’ s Dept. of Nutrition, under the direction of Penny Kris-Etherton, Distinguished Professor, looked at 10 men and 13 women aged between 21 and 62, who ate one of two experimental diets for 4 weeks. Half were allocated an average American diet altered to be low in flavonoids, while the remaining participants followed a diet containing about 22 g of cocoa powder and 16 g of dark chocolate per day.
They then ate their normal diet for a 2-week break period, before switching to consume the experimental diet they hadn’t already tried for another 4-week period.
The scientists then evaluated and compared LDL susceptibility to oxidation while the participants were on each diet. According to the paper, “The incorporation of dark chocolate and cocoa powder into the diet is one means of effectively increasing antioxidant intake. Furthermore, the inclusion of dark chocolate and cocoa powder in a diet that is rich in other food sources of antioxidants, such as fruits, vegetables, tea and wine, results in a high antioxidant intake and may consequently reduce the risk of cardiovascular disease.”
The study found that while eating the diet containing cocoa and chocolate, oxidation in the subjects’ bodies occurred about 8% slower than when they ate the experimental average American diet.
Participants gave blood at the end of each diet period, and the researchers found that total antioxidant capacity and HDL cholesterol were both 4% higher after consuming the diet containing cocoa and chocolate than after consuming the average American diet.
Chocolate, garlic, or avocado oil may not be the single preventive cure for CVD. The best preventive medicine to date is still a balanced diet and adequate exercise. Kritchevsky’s main advice for consumers is moderation. The onus is on them.
by LINDA MILO OHR
Contributing Editor
Chicago, Ill.


