Food Scientists & Dietary Reference Intakes: An Important Alliance
Regular updating of the Dietary Reference Intakes is integral to effective health and nutrition strategies.

The Dietary Reference Intakes (DRIs) are a set of common nutrient standards set by the Food and Nutrition Board (FNB) of the Institute of Medicine (IOM). The IOM has been setting nutrient standards for the United States since 1943; they are a benchmark for nutritional adequacy in the United States and Canada (IOM, 2006b). As such, they support many program, policy, and regulatory initiatives. For example, federal guidance based on the Dietary Guidelines for Americans available to consumers through the 12 energy patterns accessed through MyPlate.gov are based on food modeling to achieve intakes of essential nutrient values of the DRIs. Government programs that support food assistance such as lunch and breakfast for school-age children and nutrition for the elderly must meet the recommendations of the Dietary Guidelines for Americans and, therefore, the DRIs. Food labels report amounts of essential nutrients provided by each serving relative to nutrient recommendations from the IOM.
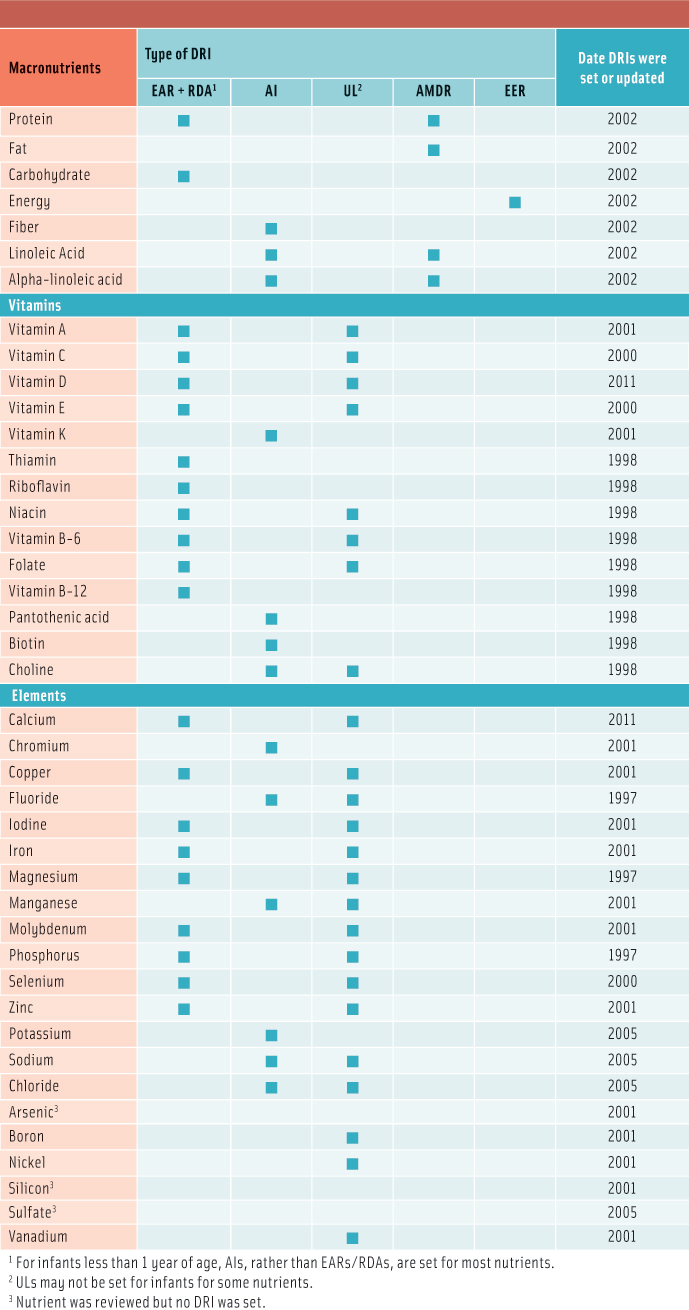
Maintaining current nutrient recommendations based on evolving science is critical to the health of the nation. Not only are they the basis for the goals of food programs and labeling in North America; they provide the reference for determining nutrient adequacy of populations, the basis for giving public health advice and dietary guidance to individuals, and goals for food product development. The IOM designated DRIs for 35 essential nutrients between 1997 and 2005 (IOM, 2007). Since then, the IOM has updated only calcium and vitamin D (IOM, 2011b). This rate of updating is woefully inadequate. Rather than a regular evaluation of all nutrients, there was a recent call for nominations for nutrients to update in the Federal Register (USDA and HHS, 2013). Despite the great response, it is unlikely that any nutrients will be revised in the coming year. There is no congressionally mandated budget to update the DRIs on a regular basis as there is for the dietary guidelines, which are updated every five years. Without updated DRIs for nutrients, there is lack of direction from new research to alter food guidance for meeting nutrient needs. The current financial climate restricts the support of government agencies necessary for optional projects such as updating the DRIs. The DRIs are important to the activities of food scientists and nutritionists and the food and supplement industries.
--- PAGE BREAK ---
What Is the Purpose of DRIs?
DRI standards are based on scientifically grounded relationships between nutrient intakes and indicators of adequacy as well as the prevention of chronic diseases in healthy populations. DRIs exist for infants, two age groups of children, 12 age/sex groups of adults, and pregnant and lactating women. This information is essential for assessing the nutritional adequacy of dietary intakes and may also be used to plan nutritious diets (IOM, 2000, 2003). Some uses of the DRIs are for individuals (such as selecting appropriate food-based dietary guidelines) while other uses are for population groups (such as evaluating dietary data from national surveys).
 For most nutrients, a single standard, the Recommended Dietary Allowance (RDA), was used for many different purposes. However, in 1994 the IOM recognized that there were many limitations to the full use of these standards and subsequently set DRIs (IOM, 1994). An RDA is simply a target intake that should be adequate for almost everyone; it does not describe the actual distribution of requirements within a population. In particular, RDAs increased the likelihood of overestimating the magnitude of a nutritional problem. DRIs nullify this issue by providing both an estimated average requirement (EAR) and its standard deviation for most micronutrients. As a result, statistical theory can be applied to better estimate the true prevalence of inadequacy within a population. In addition, an RDA is defined and can be used as the target intake for an individual and as the basis for nutrient standards on food labels.
For most nutrients, a single standard, the Recommended Dietary Allowance (RDA), was used for many different purposes. However, in 1994 the IOM recognized that there were many limitations to the full use of these standards and subsequently set DRIs (IOM, 1994). An RDA is simply a target intake that should be adequate for almost everyone; it does not describe the actual distribution of requirements within a population. In particular, RDAs increased the likelihood of overestimating the magnitude of a nutritional problem. DRIs nullify this issue by providing both an estimated average requirement (EAR) and its standard deviation for most micronutrients. As a result, statistical theory can be applied to better estimate the true prevalence of inadequacy within a population. In addition, an RDA is defined and can be used as the target intake for an individual and as the basis for nutrient standards on food labels.
Importantly, the DRIs include a tolerable upper intake level (UL) for many nutrients. The UL has been particularly helpful in counseling individuals to avoid excessive nutrient intakes—particularly from supplements and fortified foods—while providing guidance to the food and supplement industries about levels of nutrients in their products. Other types of DRIs are set for certain nutrients. For example, when there is insufficient evidence to set an EAR and an RDA, an adequate intake is used as the nutrient standard. In some ways, adequate intakes are like the older RDAs in that they are not based on a mean and standard deviation of a requirement. Thus, it is not possible to accurately estimate a prevalence of inadequacy for nutrients with an adequate intake.
Two other types of DRIs are used for energy requirements and the desirable ranges of macronutrient intakes (IOM, 2005). For energy intake (i.e., calories), equations have been developed to calculate an individual’s estimated energy requirement (EER) based on age, sex, height, body weight, and activity level. The EER is the average energy intake that will maintain a person’s body weight over time. The acceptable macronutrient distribution range (AMDR) is a guide to the healthy distribution of calories consumed as protein, fat, and carbohydrate. For adults, AMDRs are 20%–35% of calories from fat, 10%–35% of calories from protein, and 45%–65% of calories from carbohydrate.
--- PAGE BREAK ---
Who Uses DRIs?
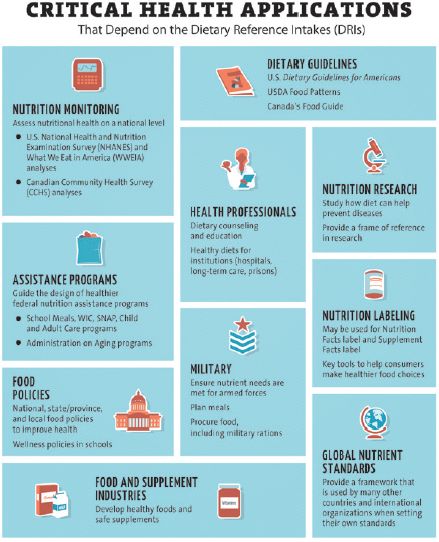
Numerous health applications depend on the DRIs, but nine are especially critical for healthy Americans and Canadians:
Nutrition monitoring. The Centers for Disease Control and Prevention spends considerable time and resources conducting the ongoing National Health and Nutrition Examination Survey (NHANES), which includes a dietary component, “What We Eat in America.” The agency collects two days of dietary data from a representative sample of approximately 5,000 Americans every year. A key use of these dietary data is to estimate intakes of 65 nutrients and then evaluate them relative to the DRIs. Nutrients of concern are identified when substantial proportions of the American population report intakes that are too low or too high (Moshfegh et al., 2005). In turn, this information is used to guide a variety of nutrition policies and programs. If DRIs are not current, then it becomes difficult to correctly identify priorities for future efforts.
Dietary guidelines. The DRIs furnish reference standards for nutrients; however, most dietary guidance provides recommendations for intake of foods. Thus, the U.S. Dept. of Agriculture (USDA) revises the Dietary Guidelines for Americans every five years to provide practical guidance on choosing healthy food patterns for adults and children ages 2 and older (USDA and HHS, 2010). Based on the dietary guidelines, as well as the DRIs, the USDA has developed recommended intakes from 13 food groups across 12 levels of energy intake ranging from 1,000 kcal/day to 3,200 kcal/day (USDA, 2012).
Importantly, following these foods patterns will help consumers meet or exceed almost all of the RDAs and adequate intakes for nutrients. All federal nutrition programs must conform to the dietary guidelines, and nutrition education programs are built on them. It is therefore particularly unfortunate that while the dietary guidelines are revised every five years by congressional mandate, the nutrient standards on which they rely may be considerably out of date (see Table 1).
 Health professionals. Registered dietitians and other healthcare professionals rely on nutrient standards when counseling patients and clients. A wide variety of software has been developed to assist in evaluating an individual’s diet and providing quick results that are then used to suggest dietary changes, if needed. These programs rely on DRIs not only to assess dietary intakes but also to assist dietitians in educating consumers and making recommendations for dietary changes. Other types of computer programs are used to plan healthy diets for specific groups, such as people residing in hospitals or long-term care facilities. These programs also rely on DRIs. It is obvious that DRIs need to be current, or the risk of giving incorrect advice or planning unhealthy programs is increased.
Health professionals. Registered dietitians and other healthcare professionals rely on nutrient standards when counseling patients and clients. A wide variety of software has been developed to assist in evaluating an individual’s diet and providing quick results that are then used to suggest dietary changes, if needed. These programs rely on DRIs not only to assess dietary intakes but also to assist dietitians in educating consumers and making recommendations for dietary changes. Other types of computer programs are used to plan healthy diets for specific groups, such as people residing in hospitals or long-term care facilities. These programs also rely on DRIs. It is obvious that DRIs need to be current, or the risk of giving incorrect advice or planning unhealthy programs is increased.
Nutrition research. Researchers investigating links between diet and diseases often use nutrient standards to design intervention studies. DRIs provide a scientifically based range of appropriate intakes to use in these studies, typically between the RDA and the UL. Likewise, these standards can provide a frame of reference to help researchers interpret associations that are seen in observational studies. This research can influence the need to revise the DRIs in the future as links between diet, health, and disease become better understood. Given the pace of new findings from scientific studies on nutrition and health outcomes, it is reasonable to expect that DRIs can quickly become outdated.
Assistance programs. Food assistance programs are designed to provide healthy foods to America’s most vulnerable populations: low-income families, children, pregnant and lactating women, and elderly or disabled adults. To be effective, these programs must address nutritional problems unique to these groups, and DRIs play an important role in identifying nutrients of concern. The IOM has issued recommendations for three of the large food assistance programs administered by the USDA: Special Supplemental Nutrition Program for Women, Infants, and Children (WIC); school meals; and child/adult day care (IOM, 2006a, 2009, 2011a). The IOM relied on DRIs to interpret dietary data for the target populations and identify changes needed to improve the nutritional value of the programs. Up-to-date DRIs are crucial to keep the quality of food assistance programs high.
--- PAGE BREAK ---
Food policies. Policies related to food and nutrition are set by many agencies and organizations at local, state, and national levels. For example, policies related to sugar-sweetened beverages have been implemented by many school districts and certain cities. These and other food policies should be informed by scientific research on the role of nutrition in promoting health and preventing diseases. Nutrient standards such as DRIs should feature prominently when selecting such nutrition policies. Current DRIs would ensure that consistent policies are implemented across many stakeholders.
Military. Meeting the nutrient needs of military personnel is essential to maintain the health and numbers of the country’s armed forces. Indeed, the need for nutrient standards in the United States was first implemented in order to ensure healthy soldiers during World War II. Applications of DRIs within the military include planning nutritious meals in canteen services on bases, ensuring healthy field rations, and designing appropriate food procurement systems.
Nutrition labeling. An important component of nutrition education for consumers is the information that is found on the Nutrition Facts Label and the Supplement Facts Label. The daily values (DVs) that are used on these labels are derived from nutrient standards and provide consumers with a guide to compare and evaluate the nutrients in various products. Although the current DVs specified by the U.S. Food and Drug Administration are based on the older RDAs, the agency recently released a proposed approach to updating the DVs so that they would use newer DRIs (FDA, 2014). Front of package nutrition information is also typically based on nutrient standards. Current DRIs would allow consumers to access the best possible nutrition information to help guide their purchases.
Food and supplement industries. Food products are often developed and marketed to meet consumers’ preference for healthy foods. Consumers have become more aware of the importance of nutritious foods. Furthermore, restrictions on the types of foods provided in federal food assistance programs such as school meals and WIC have led to the development of many new products that meet healthy criteria. The DRIs drive many of these trends directly through consumer awareness and indirectly through food labeling and the Dietary Guidelines for Americans. Dietary supplement manufacturers are also aware of the importance of consumer knowledge and develop products to meet perceived needs. A new aspect of the DRIs, the setting of ULs for many nutrients, provides a way to evaluate whether supplements (and fortified foods) are providing nutrients in excessive amounts. Without up-to-date DRIs, manufacturers could develop products that ultimately do not address correct health outcomes.
 Why Should DRIs Be Revised Regularly?
Why Should DRIs Be Revised Regularly?
Many of the DRIs for children are derived from adult requirements or from other age groups of children and should be re-examined. Although this approach is necessary when requirement data are unavailable, it has sometimes led to unrealistic values for both requirements and upper levels. For example, 69% of children ages 1–3 and 22% of those ages 4–8 years reported intakes above the zinc UL of 7 mg/day and 12 mg/day, respectively, in NHANES data from 001–2002 (Moshfegh et al., 2005). Yet there is no evidence of zinc toxicity, seen as compromised copper metabolism, in these age groups. The process of deriving the zinc UL for young children from the adult UL led to an unrealistic UL for the children. Adequate intakes (AIs) have limited uses and should be replaced with EARs and RDAs. AIs were originally used only to set DRIs for infants; because infant requirements are based on the nutrient content of breast milk, an EAR and its standard deviation are unknown. However, AIs have also been used to express the requirements of other age groups (see Table 1), thus severely limiting their applications. For nutrients with an adequate intake, it is not possible to estimate the prevalence of inadequate intakes and thus impossible to rank the magnitude of concern about possible inadequacies.
Whenever conceivable, AIs should be eliminated as was done for adults and children when the DRIs for calcium and vitamin D underwent revision in 2011. Better methods for setting the ULs have been proposed and should be evaluated. The risk assessment model has been valuable, but there has been little work on the possibility of estimating a risk curve for excessive intakes that mirrors the requirement curve used to determine an EAR and its standard deviation. As a result, ULs must be used as a cut-point. Newer science may show that some of the DRIs are incorrect. For example, researchers have argued that the EARs and RDAs for vitamin E are too high (Devaney et al., 2006). The prevalence of inadequacy for vitamin E is estimated to be 89% for males 19 years and older and 97% for adult females based on intakes reported in 2001–2002 NHANES data (Moshfegh et al., 2005). However, clinical signs of such widespread deficiencies are not present. The adult requirement is based on the prevention of hydrogen peroxide-induced hemolysis, but it is possible that a more relevant outcome should be identified. Vitamin E also provides an example of the problems in extrapolating DRI values from one age group to another: Children’s requirements are based on those for adults after adjusting for differences in body sizes resulting in similar inadequacies. For all nutrients that have DRIs, new science has explored their roles in health and disease since their DRIs were originally set. A similar explosion of new data on requirements and toxicity has occurred for many other nutrients. In addition to a revision process for essential nutrient DRIs, standards for intakes of other bioactive compounds (e.g., non-essential compounds) need to be considered. Methods for setting such standards should be explored, and a discussion of the types of standards that would be appropriate should be initiated (Biesalski et al., 2013).
--- PAGE BREAK ---
A Call to Action
Two processes have been proposed as ways to timely update DRIs, but neither will ensure a systematic review of all nutrients on a regular basis. The first process is established through a DRI subcommittee of the U.S. and Canadian governments. This process applies only to nutrients that currently have DRIs. The first call for comments was published in the Federal Register, and nominations for nutrients were accepted May–June 2013. Submissions were received for 16 nutrients, of which four were selected for further consideration. However, funding was not allocated for a comprehensive review of any of these nutrients. Thirty-five nutrients have DRIs, so if one or two nutrients were selected annually, the process would take decades. There is no proposal for routine evaluation of all nutrients, and there is no consideration being given to nonessential nutrients.
The second proposal is by the FNB. In this process, a core FNB committee would conduct a periodic review of all DRI values to establish whether new evidence is sufficient to trigger a deeper, systematic review. The FNB committee would serve as an interface to the government nomination process for major updates. The FNB core committee could perform minor changes to the existing DRI reports as part of the triage process. These could include updates in population intakes or revisions of a particular population subgroup. The FNB is using two nutrients, thiamine and phosphorus, as a model to develop the evaluation process. Development of an approach to update the DRIs that reduces costs but retains scientific rigor is the goal.
The problem with the current and two proposed processes is lack of funding. This creates a critical gap for all of the applications of the DRIs. How can the dietary guidelines committee assemble and interpret accurate literature referenced against outdated nutrient standards? A movement calling for a mandate to regularly update the DRIs is one of the most urgent efforts toward a healthier diet.
Connie Weaver, Ph.D., a Member of IFT, is Distinguished Professor and Dept. Head, Nutrition Science, at Purdue University, West Lafayette, IN ([email protected]).
Suzanne P. Murphy, Ph.D., R.D., is Nutrition Researcher Emeritus, Univ. of Hawaii Cancer Center, Honolulu, HI ([email protected]).
References
Biesalski, H.K., Erdman, J.W., Hathcock, J., et al. 2013. Nutrient reference values for bioactives: new approaches needed? Eur. J. Clin. Nutr. 52: 1–9.
Devaney, B., Crepinsek, M.K., Fortson, K., and Quay, L. 2006. Review of the dietary reference intakes for selected nutrients: Application challenges and implications for food and nutrition assistance programs. Mathematica Policy Research, Princeton N.J. http://www.mathematica-mpr.com/publications/PDFs/dietaryreference.pdf.
FDA. 2014. U.S. Food and Drug Administration: Proposed changes to the nutrition facts label. http://www.fda.gov/food/guidanceregulation/guidancedocumentsregulatoryinformation/labelingnutrition/ucm385663.htm.
IOM. 1994. Institute of Medicine: How Should the Recommended Dietary Allowances Be Revised? The National Academies Press, Washington, D.C.
IOM. 2000. Institute of Medicine: Dietary Reference Intakes: Applications in Dietary Assessment. The National Academies Press, Washington, D.C.
IOM. 2003. Institute of Medicine: Dietary Reference Intakes: Applications in Dietary Planning. The National Academies Press, Washington, D.C.
IOM. 2005. Institute of Medicine: Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). The National Academies Press, Washington, D.C.
IOM. 2006a. Institute of Medicine: WIC Food Packages: Time for a Change. The National Academies Press, Washington, D.C.
IOM. 2006b. Institute of Medicine: Dietary Reference Intakes, the Essential Guide to Nutrient Requirements. The National Academies Press, Washington, D.C.
IOM. 2007. Institute of Medicine: The Development of DRIs 1994–2004: Lessons Learned and New Challenges. Workshop Summary. The National Academies Press, Washington, D.C.
IOM. 2009. Institute of Medicine: School Meals: Building Blocks for Healthy Children. The National Academies Press, Washington, D.C.
IOM. 2011a. Institute of Medicine: Child and Adult Care Food Programs: Aligning Dietary Guidance for All. The National Academies Press, Washington, D.C.
IOM. 2011b. Institute of Medicine: Dietary Reference Intakes for Calcium and Vitamin D. The National Academies Press, Washington, D.C.
Moshfegh, A., Goldman, J., and Cleveland, L. 2005. What We Eat in America, NHANES 2001-2002: Usual nutrient intakes from food compared to dietary reference intakes. U.S. Dept. of Agriculture, Agricultural Research Service. http://www.ars.usda.gov/SP2UserFiles/Place/12355000/pdf/0102/usualintaketables2001-02.pdf.
USDA. 2012. U.S. Dept. of Agriculture: MyPlate. http://www.choosemyplate.gov/.
USDA and HHS. 2010. U.S. Dept. of Agriculture and U.S. Dept. of Health and Human Services: Dietary Guidelines for Americans, 2010. 7th edition. U.S. Government Printing Office, Washington DC.
USDA and HHS. 2013. U.S. Dept. of Agriculture and U.S. Dept. of Health and Human Services: Nomination for new dietary reference intakes. http://health.gov/dri/.
