Rutgers Researchers Explore the Wonderful World of Lipids
INSIDE ACADEMIA

 Over the years, scientists have held onto the promise—and socialites, the hope—that one day the holy grail of prescription drugs would exist: a fat pill—the pill that would either prevent consumers from absorbing too much fat or prevent consumers from storing fat and gaining weight. Alas, that pill has never been developed and likely never will. Researchers at the Rutgers University Center for Lipid Research know why. “Everyone is always worried about obesity,” says George Carman, director of the Center for Lipid Research and a food science professor. “What I have learned over the last 10 to 12 years is that we cannot prevent making fat. It’s crucial to make fat.” Through a multidisciplinary approach to studying fat and other lipids, Carman and his colleagues are uncovering the biochemical, cellular, and molecular mechanisms involved in lipid metabolism and the many reasons why lipids are essential to health and well-being.
Over the years, scientists have held onto the promise—and socialites, the hope—that one day the holy grail of prescription drugs would exist: a fat pill—the pill that would either prevent consumers from absorbing too much fat or prevent consumers from storing fat and gaining weight. Alas, that pill has never been developed and likely never will. Researchers at the Rutgers University Center for Lipid Research know why. “Everyone is always worried about obesity,” says George Carman, director of the Center for Lipid Research and a food science professor. “What I have learned over the last 10 to 12 years is that we cannot prevent making fat. It’s crucial to make fat.” Through a multidisciplinary approach to studying fat and other lipids, Carman and his colleagues are uncovering the biochemical, cellular, and molecular mechanisms involved in lipid metabolism and the many reasons why lipids are essential to health and well-being.
The Wide World of Lipids
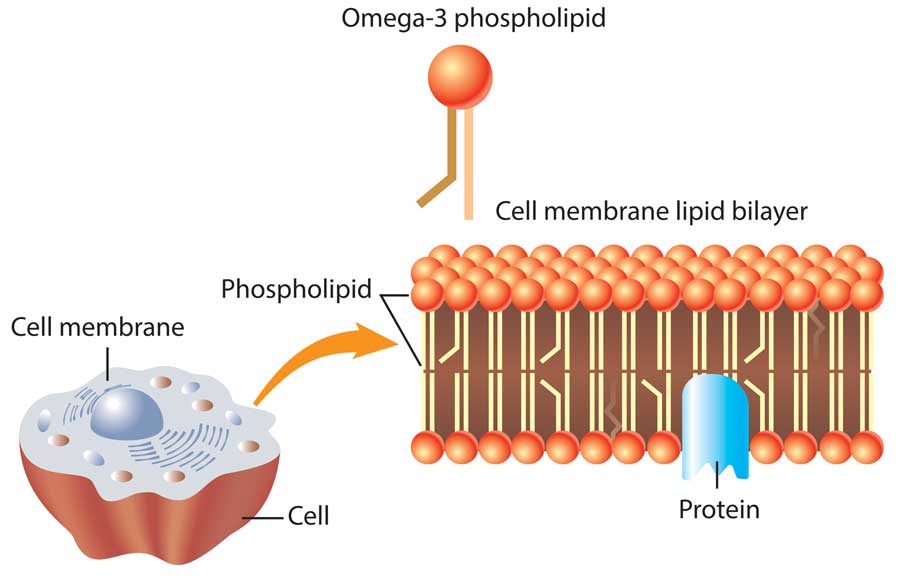
Lipids are a diverse group of organic fatty, oily, or wax-like substances that are present in humans and other organisms and responsible for a number of important functions. Most of the lipids humans consume through dietary intake are triglycerides. Triglycerides provide insulation to control body temperature and padding to protect internal organs, constitute the body’s sole form of stored energy, and aid in the metabolism of certain vitamins. Other types of lipids include fatty acids, lipoproteins, steroids (e.g., cholesterol, estrogen, and testosterone), and phospholipids, and each has different roles in the body: Fatty acids such as alpha-linolenic acid, docosahexaenoic acid, and eicosapentaenoic acid play structural roles in brain cells, nerve cells, and retinal cells and possess anti-inflammatory properties that fight disease; other fatty acids are the precursors to triglycerides and phospholipids. Lipoproteins transport other lipids, especially hydrophobic ones such as triglycerides and cholesterol, through the bloodstream. Steroids such as cholesterol and fat-soluble hormones are necessary for cell repair, the formation of new cells, and the regulation of important biological functions in the body. And phospholipids form the membranes that allow each and every cell to exist. Collectively, these and other lipids enable the body to function properly and determine far more than whether or not a person is obese. But before they can exhibit their useful properties, dietary fats must be digested and metabolized.
 Metabolizing Lipids
Metabolizing Lipids
Digestion of dietary fat begins in the mouth and stomach but occurs predominantly in the small intestine, which is the principal site for triglyceride digestion and nutrient absorption. Lipases (enzymes) and bile acids in the small intestine assist in breaking down triglycerides into monoglycerides and fatty acids. These molecules are absorbed into intestinal cells, where they are reformed into triglycerides and combined with cholesterol, phospholipids, proteins, and fat-soluble nutrients to form chylomicrons, a type of lipoprotein. “Lipoproteins are the taxicabs that deliver lipids to wherever they need to go in the body,” explains Joseph Dixon, an associate professor of nutritional sciences at Rutgers and a member of the Center for Lipid Research. “Blood is water—mostly aqueous. Oil and water don’t mix, so how do you transport oil through water? Lipoproteins. … In most cases, a lipoprotein is a spherical molecule, and it has a lipid core; therefore, it can be transported through aqueous blood.” Chylomicrons from the small intestine travel through the blood, dropping off lipids to sites in the body that need them. This process ensures not only that fat is stored in cells for energy but also that other hydrophobic lipids are delivered where they are needed. One such hydrophobic compound is vitamin A: Vitamins A, D, E, and K, which the body could not absorb without dietary fat, are lipids. These vitamins “are defined as fat-soluble because they are not mixable with water. They are hydrophobic, so they need some kind of transport system to be carried around in the body, especially in an aqueous-based system like the bloodstream,” says Loredana Quadro, an associate professor of food science at Rutgers and a member of the Center for Lipid Research. These fat-soluble vitamins are also essential micronutrients. “Essential micronutrients are micronutrients that we cannot synthesize, so we have to obtain them from the diet.” Preformed vitamin A is in eggs, fish, meat, poultry, and dairy products. Provitamin A—the carotenoids alpha-carotene, beta-carotene, and beta-cryptoxanthin—are found in green, orange, and yellow vegetables and fruits such as apricots, broccoli, cantaloupe, carrots, dark leafy greens, squash, sweet potatoes, and tomatoes. Beta-carotene is the most common provitamin A carotenoid in foods and dietary supplements; other well-known carotenoids such as lycopene, lutein, and zeaxanthin are not converted to vitamin A. “We ingest the vitamin A, and then it gets into the intestines, and because it comes from food, it is either in the form of retinol and retinyl ester from foods from animal sources, ... or it’s in the form of precursors, which many come from fruits and vegetables,” Quadro says. “We know [vitamin A] is good for vision; we might know that it’s good for skin. But vitamin A does a lot of other stuff.”
Vitamin A is imperative for normal vision, reproduction, fetal development, wound healing, bone formation, and hair growth; it also helps protect against infections in the digestive, respiratory, and urinary tracts. Moreover, because of its role in maintaining a normal immune system, vitamin A is frequently referred to as the anti-infective vitamin. Quadro, who studies the metabolism of vitamin A and all of the important roles it plays in the body, points out another extraordinary function of this micronutrient: “[Vitamin A] performs transcriptional regulatory activity. [It] can actually impact the way our DNA releases information. … So this is one of the examples of food components that can actually impact health by acting, if you will, by modifying the activity of our genome. … This is a function we don’t think about when we think about food.”
Vitamin A deficiency is the most prevalent vitamin deficiency in the world. It is the leading cause of preventable blindness in children; other manifestations of vitamin A deficiency are chronic illness caused by persistent low resistance to infections, dry skin and hair, and spontaneous miscarriages. “There are literally millions of people that are affected by vitamin A deficiency despite a lot of programs to overcome this burden that mainly affects underdeveloped countries,” Quadro emphasizes. “Most of the kids that are severely deficient in vitamin A, which are the ones who go blind, will probably die from an infectious disease within six months of losing their eyesight. … There is also a lot of research that is starting to discover that even in the Western world, although we may tend to eat too much vitamin A, there are instances in which people may be prone to develop some kind of [vitamin A] deficiency—maybe not systemic but in some peripheral tissues.” According to Quadro, whose research also involves the transfer of vitamin A from mother to fetus, there is evidence to suggest that vitamin A deficiency can also cause congenital malformations such as cleft face and cleft palate.
Cholesterol: Friend or Foe?
While everyone can appreciate the importance of vitamin A, most people rarely appreciate the importance and necessity of cholesterol and lipoproteins. This is because these molecules are most often associated with poor health and increased risk of adverse cardiovascular events. Cholesterol “is an extremely important molecule,” declares Dixon, whose laboratory conducts research on cholesterol, low-density lipoproteins (LDLs), and very low-density lipoproteins (VLDLs). “It’s an ancient molecule; you’ll find it in many different kinds of ancient creatures. … Cholesterol is the cinderblock of the cell membrane,” he adds. “Animal cells have to have cholesterol to keep their membranes strong and structured. Without the cholesterol, the fatty acids would just be wiggling all over.” Cholesterol is also the precursor of steroid hormones. “Testosterone, estrogen, cortisol, progesterone, [and] vitamin D are all made from cholesterol, and bile acids are made from cholesterol,” Dixon pronounces. “And the neurons in the brain have a cholesterol sheath around them, and that provides insulation—it’s almost like electrical tape around the axon. So without cholesterol, we’d be in bad shape.” LDLs transport cholesterol, which is hydrophobic, from the liver through the bloodstream to cells that need it while high-density lipoproteins (HDLs) clear cholesterol from areas where too much of it has been deposited and return it to the liver. “HDL is the body’s vacuum cleaner for cholesterol,” Dixon asserts. And VLDLs carry triglycerides, delivering them to cells in the body. Central to this lipid metabolism is the liver; it secretes VLDLs, which form LDLs, and HDLs—thereby synthesizing cholesterol for export to other cells but also removing it from the body.
The lipid metabolism system continues all day every day. It cannot stop; if it did, the heart would stop. “The heart uses a lot of energy, and if it used glucose, you wouldn’t have glucose for the brain or enough for the muscles,” Dixon explains. “Ninety-five percent of the substrate for the heart is free fatty acids.” Normally, the lipid metabolism system works fine for up to about 50 years, but then it begins to behave abnormally, which leads to a number of fat-related diseases. “This system, which is absolutely necessary to keep us alive, goes a little haywire once we get older,” Dixon says, because “there are receptors in the liver that take up the excess LDL. And just like anything in any human, when you age, you start to lose things: muscle, fibers, neurons, nice smooth skin. Like anything else, the LDL receptors in the liver go down with age, and therefore, the blood LDL goes up with age.” When this happens, more LDLs can become lodged in blood vessels, leading to cardiovascular disease and other health issues. “If you can trick the liver into thinking it needs cholesterol by inhibiting the synthesis of cholesterol in the liver, it up-regulates its LDL receptors and the [level of] LDL comes down,” Dixon says. This is what the drugs Lipitor, Pravastatin, and Simvastatin were designed to do, but most consumers can control their cholesterol levels through diet. “After someone’s basic genetics, saturated fat and lack of fiber are two important determinants of blood cholesterol in the body,” Dixon reveals. “It turns out that saturated fat, for some reason we don’t know, negatively affects the LDL receptors. … And that increases blood cholesterol. The second thing is that … we are consuming one-third the fiber that we evolved eating.” Dietary fiber in plant foods such as apples, barley, beans, carrots, oats and other whole grains, and psyllium lower LDL levels by binding to bile acids and cholesterol in the intestine and ushering them out of the body, thereby lowering the amount of fat and cholesterol absorbed in the body.
Phospholipid Philosophy
Cholesterol is not the only molecule in lipid metabolism that can be both friend and foe. “We’re always concerned about obesity, but we don’t think about the flipside,” Carman says. “In our diet, we take in food. One of the things that comes along for the ride are fatty acids. Fatty acids are precursors to membrane phospholipids and triglycerides (fat), but free fatty acids are very bad. How our bodies cope with free fatty acids is they get incorporated into fat.” The metabolism of fatty acids into triglycerides and other lipids is crucial to normal functioning of the human body, “and the imbalance of any of this metabolism leads to human diseases,” Carman says. Free fatty acids circulating in the bloodstream raise the risk of cardiovascular disease, metabolic syndrome, and type 2 diabetes. Carman has been studying lipid metabolism for nearly 40 years, focusing primarily on membranes and the phospholipids that form them. “All of my research has been trying to understand the underpinnings of the structure and function of membranes to figure out how they work because they’re so important,” Carman explains. Using the yeast Saccharomyces cerevisiae as a model for eukaryotic organisms, Carman and his laboratory staff have determined that during the active phase of growth (i.e., exponential phase) of yeast, cells are not making fat; they’re making membrane phospholipids so that the cells can continue to divide and grow. Carman reveals that when cells are still young, the phosphatidic acid in them is more involved with making membrane phospholipids to generate new cells. But when cells get older, the phosphatidic acid switches to making triglycerides (fat) almost exclusively. This may explain why many people can eat whatever they want while they’re young and stay slender, but around age 50 or so, they begin putting on weight unless they are very mindful of the amount and types of food they consume. Whether the body uses phosphatidic acid to make fat or cell membranes is determined by one factor: the enzyme phosphatidic acid phosphatase. Phosphatidic acid phosphatase catalyzes the next to last step in producing fat. “A lot of times in metabolic pathways,” Carman says, “it’s not the last step that’s so important; it’s the step before the last that plays a crucial role.”
Having determined the key role of phosphatidic acid phosphatase in lipid metabolism, Carman and the researchers in his laboratory set about finding the gene—essentially, the “fat gene”—that codes for the enzyme. The implications of finding that gene were enormous: identifying that gene would be the first step in the direction of finding a way to prevent the conversion of phosphatidic acid into fat. “The idea was, if we had the gene that makes fat, we’re going to come up with a pill that can prevent people from becoming obese,” Carman says. In 2006 he and his research team found the gene, PAH1, that codes for phosphatidic acid phosphatase in yeast; the gene has the same function in mammals. “So in 2006, many people in the world, including our lab, began studying this phosphatidic acid phosphatase gene [earnestly],” Carman says. Through further studies of yeast and other models, Carman’s research team and others discovered that organisms in which PAH1 was mutated or turned off made excess membrane phospholipids and had shortened lifespans from metabolic abnormalities and other causes. “You have to make fat; you don’t want to turn that enzyme off. That enzyme is crucial,” Carman emphasizes. “Making too many membrane phospholipids is bad; it may lead to inflammation, uncontrollable cell growth (cancer), and so on. … So we can’t make that pill; you don’t want to knock out that gene. What we want to do is figure out how to control or fine-tune the phosphatidic acid phosphatase enzyme.”
Carman, Quadro, and Dixon are but three of the researchers making extraordinary discoveries for the Center for Lipid Research, which is part of Rutgers University’s New Jersey Institute for Food, Nutrition, and Health. The Center for Lipid Research is comprised of more than 25 researchers who share their findings on the biochemical, biophysical, cellular, and molecular mechanisms involved in lipid metabolism and how they relate to lipid-based diseases such as obesity, cardiovascular disease, diabetes, and lipodystrophy. “It’s sort of like a focus group in lipid metabolism,” Carman declares. “In the past, the discipline of food science was involved in processing or trying to identify the components that make up the colors, flavors, and textures of foods. We know how to do that pretty well. … What we don’t know really well is some of the underpinnings.” Carman believes this information will be useful for developing new products. “There are a lot of things that are naturally found in foods that could fine-tune the metabolism, but we don’t know what they are,” Carman concludes. “Understanding … the basic metabolism of the macromolecules in food or other ingredients in food is where food science is going and where the food industry can go.” Without a doubt, Carman, Quadro, Dixon, and their colleagues in the Center for Lipid Research are making strides to open new frontiers for food science and nutrition.
Toni Tarver is senior technical editor of Food Technology magazine ([email protected]).


 Joseph Dixon, associate professor of nutritional sciences at Rutgers University, studies the metabolism of blood lipids and lipoproteins. From his years researching cholesterol and serving as a scientific advisor to pharmaceutical companies that make statins, Dixon has reached some interesting conclusions. “Throughout evolution, for most humans, the average age they died was probably 40 or 45. Now we live a lot longer, so as we grow older, the system that regulates lipoproteins kind of goes hayw…
Joseph Dixon, associate professor of nutritional sciences at Rutgers University, studies the metabolism of blood lipids and lipoproteins. From his years researching cholesterol and serving as a scientific advisor to pharmaceutical companies that make statins, Dixon has reached some interesting conclusions. “Throughout evolution, for most humans, the average age they died was probably 40 or 45. Now we live a lot longer, so as we grow older, the system that regulates lipoproteins kind of goes hayw…