Micronutrient Deficiency: A Global Public Health Issue
Techniques and innovations of modern food production help address micronutrient deficiencies around the globe.
A nutrient is a substance in food that provides nourishment for growth and sustainment of life. Two classes of nutrients are essential for humans: macronutrients and micronutrients. While every consumable food in the human diet is made of one or more macronutrients, not all dietary foods contain micronutrients. A diverse diet including vegetables, fruits, whole grains, dairy products, and seafood usually ensures that populations in developed countries consume the vitamins and minerals they need to develop properly and resist distinct diseases and conditions. However, in developing countries there is no easy access or availability of foods that naturally contain essential micronutrients. And while micronutrient deficiencies occur mostly in developing countries, the rise in individuals eating a vegan, vegetarian, Atkins, Paleo, or other restrictive diet is causing increased incidence of vitamin and mineral deficiencies in industrialized nations (Calton, 2010; Zelman, 2012). As a consequence, more than two billion people around the world experience micronutrient deficiencies. An insufficient or nonexistent intake of certain essential micronutrients can result in preventable blindness, diminished mental capacity, birth defects, chronic diseases, and even death. Which essential nutrients are most deficient in the global population, and what are some feasible solutions to micronutrient deficiencies around the world?
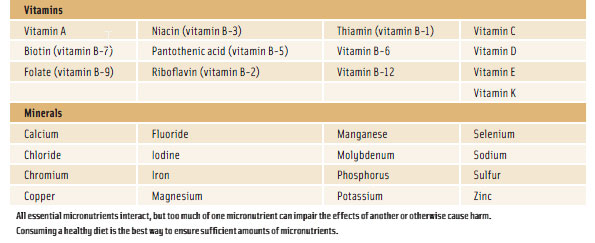
Carbohydrates, proteins, and fats—the essential macronutrients—provide energy for the body to grow, develop, and repair tissues. Water—another essential nutrient for life—aids digestion, removes waste through urine and bowel movements, assists in maintaining homeostasis, and helps distribute other nutrients to cells. Vitamins and minerals are micronutrients, which humans and other animals need in small doses to facilitate and regulate normal bodily functions and chemical reactions. Not all dietary foods contain micronutrients, so certain vitamins and minerals are obtainable only through specific foods or dietary supplements; the human body cannot synthesize them. Of the more than 20 vitamins and minerals that are essential for humans, deficiencies in folate, iodine, iron, vitamin A, and zinc are having a significant impact on public health in developing countries as well as industrialized nations.
The Deficient Five
Folate is a form of vitamin B (B-9) that is naturally present in many foods: asparagus, Brussels sprouts, dark green leafy vegetables, oranges, melons, liver, salmon, eggs, legumes, and whole grains. In addition, folic acid, the synthetic form of folate, is added to many products made from refined grains. Like all B vitamins, folate is water-soluble and helps the body convert carbohydrates into energy (glucose). Moreover, the body specifically needs folate to produce deoxyribonucleic acid (DNA), ribonucleic acid (RNA), and other genetic material; facilitate proper cell division; and form red blood cells. Another crucial role of folate is the part it plays in normal brain development and function. Individuals who are deficient in folate can experience megaloblastic anemia, decreased mental capacity, poor growth, tongue and mouth sores, and changes in the color of hair or skin. In particular, women who are deficient in folate before conception and during pregnancy are at risk of having babies with neural tube defects, such as anencephaly and spina bifida. In fact, research has determined that more than 40% of neural tube defects can be prevented by women increasing their intake of folate (CDC, 2010). The indisputable role of folate in the birth of healthy babies prompted the U.S. Food and Drug Administration (FDA) to require the addition of folic acid to bread, cereal, flour, cornmeal, pasta, rice, and other grain products sold in the United States since 1998. Scientific evidence also links the consumption of foods that naturally contain folate with a decreased risk of certain forms of cancer (NIH, 2013).
 Iodine is a non-metallic trace element that is naturally present in vegetables such as spinach, Swiss chard, summer squash, and turnip greens; fish, shrimp, and other seafood; garlic; eggs; and dairy products. The body needs iodine to make thyroid hormones, which control metabolism and are essential for normal growth and development of the brain and skeleton. Up to 80% of the iodine in the body is found in the thyroid gland in the neck, and the rest is distributed throughout the body. Iodine deficiency hinders the production of thyroid hormones, and insufficient levels of thyroid hormones can lead to thyroid issues such as goiter and hypothyroidism. It is also the most common cause of preventable brain damage around the world (NIH, 2011; WHO, 2013a). Although iodine deficiency was common in parts of the United States, Canada, and the rest of the world before the 1920s, the introduction of iodized salt in 1924 has virtually eradicated the issue in industrialized countries. Today, iodized salt is used in nearly 70% of households worldwide; it is perhaps the most successful and widely used functional food. Yet in some resource-poor regions, food sources of iodine are still scarce. For example, in industrialized countries, plant foods absorb iodine from iodine-rich soil, there is plenty of seafood that comes from oceans (the world’s most abundant source of iodine), and iodized salt is a food-supply staple. In some developing regions, however, soil has poor iodine content, there is no access to seafood, and iodized salt is unavailable. Hence, approximately two billion people around the world— close to 30% of the world’s population—have iodine deficiency (de Benoist et al., 2008).
Iodine is a non-metallic trace element that is naturally present in vegetables such as spinach, Swiss chard, summer squash, and turnip greens; fish, shrimp, and other seafood; garlic; eggs; and dairy products. The body needs iodine to make thyroid hormones, which control metabolism and are essential for normal growth and development of the brain and skeleton. Up to 80% of the iodine in the body is found in the thyroid gland in the neck, and the rest is distributed throughout the body. Iodine deficiency hinders the production of thyroid hormones, and insufficient levels of thyroid hormones can lead to thyroid issues such as goiter and hypothyroidism. It is also the most common cause of preventable brain damage around the world (NIH, 2011; WHO, 2013a). Although iodine deficiency was common in parts of the United States, Canada, and the rest of the world before the 1920s, the introduction of iodized salt in 1924 has virtually eradicated the issue in industrialized countries. Today, iodized salt is used in nearly 70% of households worldwide; it is perhaps the most successful and widely used functional food. Yet in some resource-poor regions, food sources of iodine are still scarce. For example, in industrialized countries, plant foods absorb iodine from iodine-rich soil, there is plenty of seafood that comes from oceans (the world’s most abundant source of iodine), and iodized salt is a food-supply staple. In some developing regions, however, soil has poor iodine content, there is no access to seafood, and iodized salt is unavailable. Hence, approximately two billion people around the world— close to 30% of the world’s population—have iodine deficiency (de Benoist et al., 2008).
--- PAGE BREAK ---
One of the most abundant metals on the planet and a key component in the metabolism of most forms of life, iron is a mineral that exists in two dietary forms in various foods. Heme iron, which is derived from hemoglobin, is naturally present in foods from animals that utilize hemoglobin: beef, chicken, fish, pork, liver and other organ meats, and oysters and other seafood. Non-heme iron is naturally present in certain plant foods: beans, peas, nuts and seeds, dark green leafy vegetables, and whole grains. Iron is an essential element of red blood cells, which transport oxygen to every cell in the body, as well as hundreds of human proteins and enzymes. It is also essential for the regulation of cell growth and the production of adenosine triphosphate, an energy-carrying molecule present in all living organisms. Even though the body absorbs heme iron better than non-heme iron, the latter is added to enriched and fortified foods, which is why most dietary iron is non-heme iron. Meat proteins and vitamin C help improve the body’s absorption rate of non-heme iron; tannins, poly-phenols, and calcium decrease its absorption rate. Iron deficiency is the most common nutrient disorder in the world, affecting populations in developing countries as well as those in affluent nations (WHO, 2013b). Iron-deficiency anemia (inadequate iron for the formation of normal red blood cells) is associated with both poor absorption of iron and insufficient dietary intake of iron.
Retinoids and certain carotenoids are forms of vitamin A, a fat-soluble vitamin naturally present in animal food sources and plant foods. Preformed vitamin A is in eggs, fish, meat, poultry, and dairy products. Provitamin A is found in green, orange, and yellow vegetables and fruits such as apricots, broccoli, cantaloupe, carrots, dark leafy greens, squash, sweet potatoes, and tomatoes. The most common provitamin A in foods and dietary supplements is beta-carotene, which the body converts to vitamin A; other well-known carotenoids such as lycopene, lutein, and zeaxanthin are not converted to vitamin A. Vitamin A is imperative for normal vision, fetal development, wound healing, and bone formation, and it helps protect against infections in the digestive, respiratory, and urinary tracts. Moreover, because of its role in maintaining a normal immune system, vitamin A is frequently referred to as the anti-infective vitamin. Vitamin A deficiency is rare in industrialized countries because natural sources of vitamin A and vitamin-A fortified foods are plentiful. But in developing countries—many of which have poor access to eggs, fish, dairy products, colorful produce, and fortified cereals—the leading cause of preventable blindness in children is vitamin A deficiency (WHO, 2013c). Other effects of vitamin A deficiency are an increased risk of respiratory disease and a higher risk of death from diarrhea and infectious diseases.
Another essential trace mineral for all forms of life, zinc is naturally present in beans, dairy products, nuts, whole grains, beef, poultry, and shellfish. Its bioavailability is much higher in animal foods than in plant foods. In fact, oysters contain more zinc per serving than any other food. Besides iron, zinc is the most common mineral in the human body; it is present in every cell. The ubiquitous presence of zinc in the body translates to its indispensable role in numerous cellular functions. It is involved in DNA synthesis and gene expression, cell division, protein synthesis, and the catalytic activity of more than 300 enzymes (LPI, 2013). Zinc is also required for blood clotting; normal development during gestation, infancy, and childhood; and proper vision, smell, taste, and immune function. Zinc deficiency causes arrested development in infants and children and delayed sexual development in adolescents. Hair loss, eye and skin sores, diarrhea, inadequate wound healing, and male impotence are also symptoms of zinc deficiency.
Effects of Micronutrient Deficiencies
Not only do micronutrient deficiencies in developing countries cause specific diseases such as preventable blindness and neural tube defects; they also intensify the effects of infectious and chronic diseases in populations of industrialized nations (Tulchinsky, 2010). For example, some research identifies poor maternal micronutrient intake as being a precursor to cardiovascular disease, obesity, and type 2 diabetes (Christian and Stewart, 2010; Tulchinsky, 2010). These studies indicate that zinc deficiency is common in individuals with type 2 diabetes and that folate deficiency increases the level of homocysteine in blood, which is a risk factor for cardiovascular disease. Other studies link micronutrient deficiencies in adults to cancer, illustrating that deficiencies in folate, iron, and zinc contribute to DNA damage—a biomarker related to tumor development (Ames, 2001; Eckhardt, 2006). The role of micronutrients in preventing DNA damage is complex, but evidence suggests that folate, iron, vitamin A, and zinc as well as other micronutrients are involved in regulating gene expression, synthesizing and repairing DNA, and controlling genetic mutations (Ferguson and Philpott, 2008; Arigony et al., 2013).
The indubitable correlation between micronutrient deficiencies, DNA damage, and cancer may partially explain why populations that consume diets high in vegetables and fruits—the most micronutrient dense of all foods—have a lower risk of cancer than individuals who consume little or no plant foods. In fact, most science and nutrition experts agree that consuming foods that are naturally rich in micronutrients is the best strategy to prevent or treat micronutrient deficiencies and the effects that result from this form of malnutrition. However, in the absence of an abundance of a diverse array of naturally nutritious food sources, existing methods and new advances in food fortification could be an effective way to address micronutrient deficiencies.
Strategies to Prevent Micronutrient Deficiencies
In the United States, Canada, Japan, the United Kingdom, and other industrialized nations, food fortification and enrichment programs have been in place for some time: salt is fortified with iodine; milk is fortified with vitamins A and D; and cereals and flours are enriched with folic acid, iron, and other micronutrients. Fifty countries have mandatory fortification programs for certain foods (Hermann and Obeid, 2011). These programs add nutrients or restore those that were removed or destroyed during food processing and have helped eradicate disorders stemming from micronutrient deficiencies, such as goiter and neural tube defects. Although these programs have been successful in many aspects, micronutrient malnutrition persists around the globe. The persistence of micronutrient deficiencies in areas where there is widespread availability of diverse natural food sources as well as fortified foods challenges the rationale(s) and purpose of existing fortification programs. Instead of focusing primarily on the restoration/replacement of micronutrients lost during the processing of foods, as is the premise for most large-scale food fortification, fortification programs should also analyze more closely the bioavailability and quantities of fortificants in various foods as well as how these factors affect nutrition levels of different populations. For example, populations in both developed and developing countries tend to get most of their iron in non-heme form. Forms of non-heme iron, the primary type of iron in fortified foods, are not absorbed as well as heme iron, and this is especially true in the presence of iron absorption-inhibiting nutrients such as albumin, calcium, milk proteins, polyphenols, and phytate. These factors contribute to iron bioavailability levels of 17% or less even in diverse westernized diets (Hurrell and Egli, 2010). In addition, phytate, an antioxidant phytonutrient present in whole grains and legumes, also restricts the absorption of zinc and calcium.
--- PAGE BREAK ---
 Food aid programs for developing regions tend to have a more targeted, customized approach to food fortification. Before the 1980s, aid efforts focused largely on malnutrition resulting from low energy intake (i.e., inadequate intake of protein, fats, and carbohydrates). Presently, many food aid organizations consider not only macronutrient malnutrition but also the extent of dietary monotony in each region and the nutritional status and micronutrient needs of regional inhabitants. For example, the World Food Programme distributes fortified blended foods, which are blends of partially precooked and milled cereals with added micronutrients (e.g., Super Cereal® and Super Cereal Plus®); ready to use foods, which tend to be peanut-based products fortified with vitamins and minerals (e.g., Plumpy’Sup™ and Plumpy’Doz™ by Nutriset); and micronutrient powders, which are tasteless powders containing the recommended daily intake of a range of essential vitamins and minerals that can be sprinkled on homemade food (e.g., NurtureMate™ by H.J. Heinz Co. and Nutrifer® by Sprinkles). These food products are formulated to address micronutrient deficiencies mainly in women and children.
Food aid programs for developing regions tend to have a more targeted, customized approach to food fortification. Before the 1980s, aid efforts focused largely on malnutrition resulting from low energy intake (i.e., inadequate intake of protein, fats, and carbohydrates). Presently, many food aid organizations consider not only macronutrient malnutrition but also the extent of dietary monotony in each region and the nutritional status and micronutrient needs of regional inhabitants. For example, the World Food Programme distributes fortified blended foods, which are blends of partially precooked and milled cereals with added micronutrients (e.g., Super Cereal® and Super Cereal Plus®); ready to use foods, which tend to be peanut-based products fortified with vitamins and minerals (e.g., Plumpy’Sup™ and Plumpy’Doz™ by Nutriset); and micronutrient powders, which are tasteless powders containing the recommended daily intake of a range of essential vitamins and minerals that can be sprinkled on homemade food (e.g., NurtureMate™ by H.J. Heinz Co. and Nutrifer® by Sprinkles). These food products are formulated to address micronutrient deficiencies mainly in women and children.
Such specialized food and nutrition products allow the World Food Programme, UNICEF, the Micronutrient Initiative, and other aid organizations to administer a variety of micronutrients in general or a specific vitamin or mineral, depending on the nutrition needs of subgroups of regional populations. Moreover, the products appear to have conquered the main technical challenges involved in food fortification: 1) the nutrients are delivered in forms that the human body can absorb (i.e., the nutrients are bioavailable); 2) the fortified products have no unpleasant tastes or odors that can occur by adding fortificants to food and beverages; and 3) the nutrient delivery systems are stable, preventing changes in a nutrient’s chemical composition.
Regardless of whether food fortification is performed on a mass level, as with iodized salt and vitamin-fortified milk, or is aimed at subgroups of populations, as with fortified blended foods and micronutrient powders for women and children, its success seems obvious by the decrease or elimination of disorders caused specifically by micronutrient deficiencies. Nonetheless, while acknowledging that food fortification is an effective strategy, the World Health Organization emphasizes that “[i]ncreasing dietary diversity is the preferred way of improving the nutrition of a population because it has the potential to improve the intake of many food constituents—not just micronutrients—simultaneously” and that “micronutrient-rich foods also provide a range of antioxidants and probiotic substances that are important for protection against selected noncommunicable diseases” (WHO, 2006). This may be a valid point, but deficiencies in certain micronutrients still occur in wealthy countries with extensive options of various plant and animal foods, revealing an obvious limitation of the diverse-diet approach: Just because a variety of naturally nutritious foods is available does not mean people will eat all of them. Mass education on food, nutrition, and dietary intake along with changes in behavior would help improve the diets of individuals residing in industrialized countries. However, geographic location, agricultural development constraints, and poor distribution channels likely preclude populations in resource-poor regions from ever obtaining optimal diet diversity. An emerging technology could assist in solving this conundrum: biofortification.
 Biofortification is the breeding and/or genetic engineering of plants to improve the value, variety, and bioavailability of nutrients they contain. The technique is being used to increase the presence and bioavailability of iron, provitamin A, and zinc in staple plant foods that people in developing countries primarily consume. Such regional staple crops are adequate in energy content but poor in micronutrients. Biofortification projects that are underway are iron-biofortified rice, beans, and sweet potato; zinc-biofortified wheat, rice, beans, sweet potato, and maize; provitamin-A fortified sweet potato, maize, cassava, and rice. For the most part, these projects have been received positively, but they are not without challenges that range from political to financial to agricultural to cultural. One of the main challenges of biofortified staple crops is farmer and consumer acceptance. For example, increasing the iron and zinc content of crops does not result in sensory changes, but boosting the content of provitamin A in crops results in noticeable changes in color and possibly taste (Hotz and McClafferty, 2007). Farmers may be reluctant to grow newly gold- or orange-hued crops that could be expensive to cultivate and difficult to sell, and consumers may be reluctant to purchase and eat food that looks unfamiliar and/ or tastes unusual (Meenakshi, 2009).
Biofortification is the breeding and/or genetic engineering of plants to improve the value, variety, and bioavailability of nutrients they contain. The technique is being used to increase the presence and bioavailability of iron, provitamin A, and zinc in staple plant foods that people in developing countries primarily consume. Such regional staple crops are adequate in energy content but poor in micronutrients. Biofortification projects that are underway are iron-biofortified rice, beans, and sweet potato; zinc-biofortified wheat, rice, beans, sweet potato, and maize; provitamin-A fortified sweet potato, maize, cassava, and rice. For the most part, these projects have been received positively, but they are not without challenges that range from political to financial to agricultural to cultural. One of the main challenges of biofortified staple crops is farmer and consumer acceptance. For example, increasing the iron and zinc content of crops does not result in sensory changes, but boosting the content of provitamin A in crops results in noticeable changes in color and possibly taste (Hotz and McClafferty, 2007). Farmers may be reluctant to grow newly gold- or orange-hued crops that could be expensive to cultivate and difficult to sell, and consumers may be reluctant to purchase and eat food that looks unfamiliar and/ or tastes unusual (Meenakshi, 2009).
--- PAGE BREAK ---
 Furthermore, a curiously hued biofortified crop that is also genetically modified could face even greater opposition. Conventional breeding techniques—the primary method for most biofortification projects— have been unsuccessful in producing crops of provitamin A rice, so scientists used genes from maize and a soil bacterium to engineer rice that contains beta-carotene in the edible grain. “Golden rice” has been heralded by humanitarian groups and biotechnology companies as a long-overdue intervention to help alleviate vitamin A deficiency in rice-eating populations, but critics of genetically modified organisms disagree, and national regulatory authorities have yet to approve it for consumption. Nonetheless, research and development of golden rice continues so that it can be introduced and distributed in the Philippines and Bangladesh. Test crops of other biofortified foods are being grown in Brazil, Colombia, the Democratic Republic of the Congo, India, Kenya, Mozambique, Nicaragua, Nigeria, Pakistan, Peru, and Uganda (Ortiz, 2013). All of these countries have populations that are deficient in iron, vitamin A, and zinc. Provitamin A cassava, which is bred using conventional breeding techniques, is being well-received in Kenya and Nigeria, and Brazil is demonstrating enthusiastic acceptance of biofortification by developing and testing eight different biofortified crops, including iron-biofortified beans, zinc-biofortified rice, and provitamin-A-fortified cassava (Ortiz, 2013).
Furthermore, a curiously hued biofortified crop that is also genetically modified could face even greater opposition. Conventional breeding techniques—the primary method for most biofortification projects— have been unsuccessful in producing crops of provitamin A rice, so scientists used genes from maize and a soil bacterium to engineer rice that contains beta-carotene in the edible grain. “Golden rice” has been heralded by humanitarian groups and biotechnology companies as a long-overdue intervention to help alleviate vitamin A deficiency in rice-eating populations, but critics of genetically modified organisms disagree, and national regulatory authorities have yet to approve it for consumption. Nonetheless, research and development of golden rice continues so that it can be introduced and distributed in the Philippines and Bangladesh. Test crops of other biofortified foods are being grown in Brazil, Colombia, the Democratic Republic of the Congo, India, Kenya, Mozambique, Nicaragua, Nigeria, Pakistan, Peru, and Uganda (Ortiz, 2013). All of these countries have populations that are deficient in iron, vitamin A, and zinc. Provitamin A cassava, which is bred using conventional breeding techniques, is being well-received in Kenya and Nigeria, and Brazil is demonstrating enthusiastic acceptance of biofortification by developing and testing eight different biofortified crops, including iron-biofortified beans, zinc-biofortified rice, and provitamin-A-fortified cassava (Ortiz, 2013).
Unlimited access to a diverse array of foods that naturally contain micronutrients is a luxury that facilitates adequate daily intakes of vitamins and minerals essential for health, but even individuals who have access to various dietary staples often fail to consume a balanced, healthy diet. More notably, populations in developing countries have little or no access to diverse dietary food staples that are inherently comprised of essential micronutrients. Micronutrient deficiency—from either malnutrition or under-nutrition—is the largest single contributor to disease and death around the world. Because the food industry has been successful in addressing and nearly eradicating micronutrient deficiencies in affluent countries, it is likely that existing and emerging efforts by the agricultural, food, and biotechnology industries could make significant strides in reducing micronutrient deficiencies in resource-poor countries and help save lives.
What about Vitamin D?
Recent reports indicate that vitamin D deficiency may be on the rise, but its incidence is not as pervasive as the other micronutrient deficiencies discussed in this article. Vitamin D is a fat-soluble vitamin that is essential for maintaining normal levels of calcium within the body and proper bone growth. Unlike most of the other essential vitamins and minerals, vitamin D occurs naturally in only a few foods: fatty fish such as mackerel, salmon, sardines, and tuna; fish oils; beef liver; egg yolks; and certain mushrooms. The human body can synthesize vitamin D through exposure to ultraviolet-B radiation (i.e., sunlight), and in some countries, milk, infant formula, yogurt, and a few other foods are fortified with vitamin D. The United States began fortifying milk with vitamin D in the 1930s to fight rickets, which was a significant public health issue at that time. Symptoms of vitamin D deficiency are often nonspecific but can include tiredness and achy limbs, and some vitamin-D-deficient individuals never experience any symptoms at all. Nevertheless, low serum levels of vitamin D have been implicated as a risk factor for many ailments: breast, colon, and prostate cancer; osteoporosis; type 1 and type 2 diabetes; and high blood pressure. In addition, certain groups of people are more likely to have low levels of vitamin D:
• Infants that are exclusively breastfed
• People who are lactose intolerant, vegan, or vegetarian
• People with darker skin tones
• People who never or rarely expose their skin to sunlight
• People who are obese
Sources: National Institutes of Health and Linus Pauling Institute
Toni Tarver
is Senior Writer/Editor for Food Technology magazine
[email protected]
References
Ames, B.N. 2001. DNA damage from micronutrient deficiencies is likely to be a major cause of cancer. Mutat. Res. 475(1–2): 7–20.
Arigony, A.L.V., de Oliveira, I.M., Machado, M., et al. 2013. The influence of micronutrients in cell culture: a reflection on viability and genomic stability. Biomed. Res. Int. Article ID 597282, http://www.hindawi.com/journals/bmri/2013/597282/. Accessed Oct. 2, 2013.
Calton, J.B. 2010. Prevalence of micronutrient deficiency in popular diet plans. J. Int. Soc. Sports Nutr. Vol. 7, http://www.jissn.com/content/pdf/1550-2783-7-24.pdf. Accessed Oct. 2, 2013.
CDC. 2010. Folic acid research. Centers for Disease Control and Prevention, Atlanta, Ga., http://www.cdc.gov/ncbddd/folicacid/research.html. Accessed Oct. 4, 2013.
Christian, P. and Stewart, C.P. 2010. Maternal micronutrient deficiency, fetal development, and the risk of chronic disease. J. Nutr. 140(3): 437–445.
de Benoist, B., McLean, E., Andersson, M., and Rogers, L. 2008. Iodine deficiency in 2007: Global progress since 2003. Food Nutr. Bull. 29(3): 195–202.
Eckhardt, C.L. 2006. Micronutrient Malnutrition, Obesity, and Chronic Disease in Countries Undergoing the Nutrition Transition: Potential Links and Program/Policy Implications. International Food Policy Research Institute, Washington, D.C.
Ferguson, L.R. and Philpott, M. 2008. Nutrition and mutagenesis. Annu. Rev. Nutr. 28: 313–329.
Hermann, W. and Obeid, R. 2011. The mandatory fortification of staple foods with folic acid—a controversy in Germany. Dtsch Arztebl Int. 108(15): 249–254, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3088169/. Accessed Oct. 3, 2013.
Hotz, C. and McClafferty, B. 2007. From harvest to health: Challenges for developing biofortified staple foods and determining their impact on micronutrient status. Food Nutr. Bull. 28(2): S271–S279.
Hurrell, R. and Egli, I. 2010. Iron bioavailability and dietary reference values. Am. J. Clin. Nutr. 91(5): 14,615–14,675.
LPI. 2013. Micronutrient information center: Zinc. Linus Pauling Institute, Corvallis, Ore., http://lpi.oregonstate.edu/infocenter/minerals/zinc/. Accessed Oct. 2, 2013.
Meenakshi, J.V. 2009. Biofortification. Copenhagen Consensus Center Best Practice Paper. http://www.copenhagenconsensus.com/sites/default/files/bio.pdf. Accessed Oct. 2, 2013.
NIH. 2013. Dietary supplement fact sheet: Folate. National Institutes of Health, Bethesda, Md., http://ods.od.nih.gov/factsheets/Folate-QuickFacts/. Accessed Oct. 2, 2013.
NIH. 2011. Dietary supplement fact sheet: Iodine. http://ods.od.nih.gov/factsheets/Iodine-QuickFacts/. Accessed Oct. 2, 2013.
Ortiz, F. 2013. Brazil develops ‘superfoods’ to combat hidden hunger. The Guardian, July 18, http://www.theguardian.com/global-development/2013/jul/18/brazil-superfoods-hunger. Accessed Oct. 2, 2013.
Tulchinsky, T.H. 2010. Micronutrient deficiency conditions: Global health issues. Public Health Rev. 32(1): 243–255.
WHO. 2006. The role of food fortification in the control of micronutrient malnutrition. Part 1 of “Guidelines on Food Fortification with Micronutrients,” ed. Allen, L., de Benoist, B., Dary, O., and Hurrell, R. pp. 3–37. World Health Organization Press, Geneva, Switzerland.
WHO. 2013a. Micronutrient deficiencies: Iodine deficiency disorders. http:// www.who.int/nutrition/topics/idd/en/. Accessed Oct. 2, 2013.
WHO. 2013b. Micronutrient deficiencies: Iron deficiency anaemia. http:// www.who.int/nutrition/topics/ida/en/. Accessed Oct. 2, 2013.
WHO. 2013c. Micronutrient deficiencies: Vitamin A deficiency. http://www.who.int/nutrition/topics/vad/en/. Accessed Oct. 2, 2013.
Zelman, K.M. 2012. The caveman (paleo) diet. WebMD, http://www.webmd.boots.com/diet/features/the-caveman-paleo-diet. Accessed Oct. 2, 2013.
