University of Nebraska Allergy Researchers Fight Foreign Invasions
INSIDE ACADEMIA
Watch a video about the Food Allergy Research and Resource Program at the University of Nebraska–Lincoln and the work done there to promote understanding of food allergies.
Proteins perform a wide range of vital functions in the human body that are integral for the proper formation, operation, and regulation of tissues and organs. Proteins such as collagen and hemoglobin provide structure and support for cells and transport atoms throughout the body. As hormones, proteins transmit signals to coordinate biological processes; as enzymes, they orchestrate thousands of chemical reactions that occur in cells. And as antibodies, proteins help protect the body from certain foreign particles, such as bacteria, viruses, and toxins. Thus, proteins play instrumental roles in the body’s immune system, defending against foreign invaders, but they also comprise a set of particles responsible for the invasion: food allergens. While many aspects of food allergens remain a mystery, there is a body of information about them that continues to expand. The bulk of that knowledge would not exist were it not for the Food Allergy Research and Resource Program (FARRP) at the University of Nebraska–Lincoln (UNL).
 Defining Food Allergies and Food Allergens
Defining Food Allergies and Food Allergens
A food allergy occurs when the body’s immune system recognizes a food protein as a threat. “Humans eat all kinds of foreign proteins every day, and our immune system ignores those. Even in people with food allergies, the immune system ignores 99.9% of those proteins, but for some reason, certain proteins in certain people trigger … immune responses, and that’s a food allergy,” says Steve Taylor, a professor in the department of food science and technology at UNL and co-director of FARRP. He founded the program in 1995 after years of performing research in what had been a largely ignored and underserved field. His enduring interest in scombroid fish poisoning—which occurs when tuna, mackerel, and other fish of the Scombridae family spoil, converting the protein histidine into histamine (histamine is released when a person has an allergic reaction), thereby causing an allergy-like reaction—led to Taylor’s interest in food allergens. While working at the University of Wisconsin–Madison in the late 1970s, Taylor began collaborating with staff at the university’s medical school. “At that time, there was almost no interest in food allergies,” he says. “I remember going to my first American Academy of Allergy, Asthma, and Immunology conference in San Francisco in 1981, and there was a total of five presentations at that four-day meeting on food allergies—and I gave two of them. So it wasn’t a really hot topic.” Nevertheless, Taylor’s presentation generated a lot of interest among conference attendees. “I was encouraged by the response that I got because a lot of the people that attend the allergy meeting are allergists—they’re physicians. Their response to my presentations told me that they had a lot of patients who were interested in answers, and they had almost none of the answers,” he says.
 By 1987, Taylor had earned a reputation as an expert in food allergies and food sensitivities and was splitting his time between research on food allergens and administrative duties as the new head of the food science department at UNL. This arrangement worked well until the mid-1990s, when two events caused food allergies to become more notable: 1) reports emerged of people dying from food allergies, which caught the attention of the U.S. Food and Drug Administration (FDA) and generated the recalling of foods for undeclared allergens and 2) Pioneer Hi-Bred announced plans to develop a nutritionally superior soybean that contained a gene from Brazil nuts. During a conference at which the genetically engineered soybean was introduced, Taylor asked company representatives whether the Brazil nut gene produced the Brazil nut protein that was a known allergen; they did not know. In fact, Pioneer Hi-Bred had not even considered the fact that some people were allergic to Brazil nuts. Eager to learn more about food allergies and whether their product would pose a hazard, the company contacted Taylor after the conference and offered funding for him to perform research to determine whether the Brazil nut protein, which would make soybeans a complete protein, was allergenic. “We were able to show that that particular protein from Brazil nuts was the major allergen from Brazil nuts,” Taylor says. As a result of the findings by Taylor and other UNL staff, Pioneer Hi-Bred ceased development of that soybean.
By 1987, Taylor had earned a reputation as an expert in food allergies and food sensitivities and was splitting his time between research on food allergens and administrative duties as the new head of the food science department at UNL. This arrangement worked well until the mid-1990s, when two events caused food allergies to become more notable: 1) reports emerged of people dying from food allergies, which caught the attention of the U.S. Food and Drug Administration (FDA) and generated the recalling of foods for undeclared allergens and 2) Pioneer Hi-Bred announced plans to develop a nutritionally superior soybean that contained a gene from Brazil nuts. During a conference at which the genetically engineered soybean was introduced, Taylor asked company representatives whether the Brazil nut gene produced the Brazil nut protein that was a known allergen; they did not know. In fact, Pioneer Hi-Bred had not even considered the fact that some people were allergic to Brazil nuts. Eager to learn more about food allergies and whether their product would pose a hazard, the company contacted Taylor after the conference and offered funding for him to perform research to determine whether the Brazil nut protein, which would make soybeans a complete protein, was allergenic. “We were able to show that that particular protein from Brazil nuts was the major allergen from Brazil nuts,” Taylor says. As a result of the findings by Taylor and other UNL staff, Pioneer Hi-Bred ceased development of that soybean.
 The scrapped plan to develop a new soybean along with the increase in food recalls led to other food companies raising concerns about whether their food products contained food allergens. Taylor soon found himself spending more time responding to companies’ inquiries about food allergens than performing the administrative duties of his official title. Taylor determined that there were still many unanswered questions about food allergens and that he couldn’t dedicate the time and resources to answer them because there was no funding to do so. He felt certain that food companies would be willing to fund research that would benefit them, so Taylor started FARRP in 1995 with support from seven companies and hired the late Susan Hefle as co-director. Initially focused mainly on developing analytical methods to test for allergens (because none existed at the time), the program has since expanded to include research on a variety of issues related to food allergens, including threshold doses; allergenicity assessment of existing and novel foods; the effects various processing methods have on food allergens; and with the collaboration of physicians around the world, clinical effects and responses. Each member of the FARRP faculty focuses on a different aspect of the program’s research.
The scrapped plan to develop a new soybean along with the increase in food recalls led to other food companies raising concerns about whether their food products contained food allergens. Taylor soon found himself spending more time responding to companies’ inquiries about food allergens than performing the administrative duties of his official title. Taylor determined that there were still many unanswered questions about food allergens and that he couldn’t dedicate the time and resources to answer them because there was no funding to do so. He felt certain that food companies would be willing to fund research that would benefit them, so Taylor started FARRP in 1995 with support from seven companies and hired the late Susan Hefle as co-director. Initially focused mainly on developing analytical methods to test for allergens (because none existed at the time), the program has since expanded to include research on a variety of issues related to food allergens, including threshold doses; allergenicity assessment of existing and novel foods; the effects various processing methods have on food allergens; and with the collaboration of physicians around the world, clinical effects and responses. Each member of the FARRP faculty focuses on a different aspect of the program’s research.
Allergen Thresholds and Risk
Taylor is an expert on virtually every aspect of food allergen research, but lately his attention has been directed to threshold doses and the risk of allergen exposure due to agricultural commingling. The recent massive recall of products manufactured by Frito-Lay, Hostess, Kellogg Co., and others exemplifies why research in these areas is important: Some of the affected companies issued statements indicating that their facilities did not process peanuts, yet the recalled products might contain peanut residue. This is because through agricultural commingling, foods can be contaminated with food allergens even if the allergens and the foods are not processed in the same facility. In this case, the grain may have been contaminated by peanut dust and other peanut residue left in shared transportation and storage facilities on a farm where crop rotations occur. “What we know is that peanut farmers in Georgia rotate the [peanut] crop with wheat. So they grow the peanuts, which are a legume, [and] they’re a nitrogen-fixing crop. Then they plant wheat in the other season of the year, and they don’t need to fertilize the wheat because they grew the peanuts, so the nitrogen is naturally there,” Taylor reveals.
With shared agricultural tools and facilities (i.e., agricultural commingling), the likelihood of allergen contamination increases. In such instances, the norm is to issue a comprehensive product recall. “[The] FDA was very risk averse in this case,” Taylor says, but it may be more prudent to first ascertain whether the contamination is at a level that poses a real threat to people with food allergies. “Thresholds definitely exist for each and every individual with food allergies,” Taylor says. A threshold is the maximum amount of a specific allergen that a person with food allergies can tolerate without experiencing any adverse symptoms. “The mantra of toxicology … is ‘the dose makes the poison.’ That’s true for food allergens too,” he points out. According to Taylor, there is well-documented evidence that people with food allergies have thresholds below which they do not experience adverse reactions. Allergic reactions can range from skin symptoms (redness, hives, itching, etc.) to gastrointestinal symptoms (nausea, vomiting, diarrhea) to respiratory responses (runny nose, watery eyes, sneezing, etc.); it is the respiratory responses to food allergens that can be severe or adverse (asthma and/or anaphylaxis). Taylor believes that further reducing the risk of allergen contamination is possible, but completely preventing it is not. “That’s where thresholds come into play, but [the] FDA doesn’t recognize thresholds yet. I think we’re getting to the point where they just about have to,” he asserts. “We need to recall products that are truly risky, but the ones that are very unlikely to make anyone ill should be able to stay on the market. … You have a recalled product and you get it back; you have one thing you can do with it: Bury it in some landfill. Most people could eat it; it’s perfectly good food.”
--- PAGE BREAK ---
 Joseph Baumert, co-director of FARRP and an associate professor in the department of food science and technology, also emphasizes the importance of establishing regulatory thresholds. Baumert performs safety and risk evaluations for food allergens, so threshold data help him recommend risk management strategies to food manufacturers. “We … use those threshold values to understand where … risk may lie and understand how that threshold value on a population basis may intersect with the exposure dose, which is a function of how much you eat and how much of that residue may be present,” Baumert explains. “What we’re looking at is establishing a level at which 99% of the population would be safe.” Other factors for evaluating risk are the allergenicity of each protein, dietary surveys, and consumer behavior. Altogether, these factors help establish a quantitative risk based on an understanding of the population distribution of consumption. For example, the Food Allergen Labeling and Consumer Protection Act requires that the label of a food product that contains an ingredient that is, or contains protein from, a major food allergen (eggs, fish, milk, peanut, shellfish, soy, tree nuts, or wheat) declare the presence of the allergen. However, such labeling is not required for foods that might contain such ingredients. Thus, if a nonallergenic food product with low consumption is manufactured in a facility that also processes tree nuts, then an allergen advisory statement (e.g., “may contain traces of tree nuts”) may not be necessary, but in a food product with high consumption, the advisory allergen statement may be warranted. Baumert points out that even the advisory allergen statements themselves present a risk because there is no standard of when they should appear on labels. In addition, consumers do not really know what the advisory allergen statements mean. “They may adhere to avoiding products that say ‘may contain,’ but they may ignore the ones that say ‘processed in a shared facility,’” he says. According to data FARRP has collected, products bearing either advisory allergen statement have equal probability of risk.
Joseph Baumert, co-director of FARRP and an associate professor in the department of food science and technology, also emphasizes the importance of establishing regulatory thresholds. Baumert performs safety and risk evaluations for food allergens, so threshold data help him recommend risk management strategies to food manufacturers. “We … use those threshold values to understand where … risk may lie and understand how that threshold value on a population basis may intersect with the exposure dose, which is a function of how much you eat and how much of that residue may be present,” Baumert explains. “What we’re looking at is establishing a level at which 99% of the population would be safe.” Other factors for evaluating risk are the allergenicity of each protein, dietary surveys, and consumer behavior. Altogether, these factors help establish a quantitative risk based on an understanding of the population distribution of consumption. For example, the Food Allergen Labeling and Consumer Protection Act requires that the label of a food product that contains an ingredient that is, or contains protein from, a major food allergen (eggs, fish, milk, peanut, shellfish, soy, tree nuts, or wheat) declare the presence of the allergen. However, such labeling is not required for foods that might contain such ingredients. Thus, if a nonallergenic food product with low consumption is manufactured in a facility that also processes tree nuts, then an allergen advisory statement (e.g., “may contain traces of tree nuts”) may not be necessary, but in a food product with high consumption, the advisory allergen statement may be warranted. Baumert points out that even the advisory allergen statements themselves present a risk because there is no standard of when they should appear on labels. In addition, consumers do not really know what the advisory allergen statements mean. “They may adhere to avoiding products that say ‘may contain,’ but they may ignore the ones that say ‘processed in a shared facility,’” he says. According to data FARRP has collected, products bearing either advisory allergen statement have equal probability of risk.
 Characteristics of Allergens
Characteristics of Allergens
Some consumers and advocacy groups argue that genetically engineered foods present an even greater risk of allergen exposure because they contain genetic material from other organisms or could create new allergenic proteins. Richard Goodman, a research professor in the department of food science and technology and a FARRP faculty member, refutes that concern. “We study potential food allergy in genetically engineered crops far more than we study other crops [and] other food sources,” he asserts. Goodman manages FARRP’s AllergenOnline database, which is a searchable academic peer-reviewed list of known allergenic proteins and amino-acid sequences in a database. He describes the database as a research tool for the identification of genes and proteins that may be an allergen risk as well as a safety mechanism for evaluating the potential allergenicity of genetically engineered crops and other novel foods. “Yes, you can occasionally sensitize somebody with a new protein that nobody’s had experience with. But the biggest risk … is if you take a gene that encodes a protein that is already an allergen or that is so similar to an allergen that’s already out there and has caused allergies in people,” Goodman explains. “It’s one of the most important safety tools that are used for evaluating the potential allergenicity of genetically engineered crops.” (Indeed, had the AllergenOnline database been existence in 1995, it would have sped up the discovery that Pioneer Hi-Bred’s transgenic soybean would pose a risk.)

 The similarity of food proteins to known allergens is also useful in predicting whether other novel foods (i.e., foods not commonly consumed) could pose an allergy risk. For example, in some Westernized countries, insects constitute a relatively novel food source of protein powders and flours, but they share the same characteristics of a group of foods that Westerners regularly consume. “Insects are arthropods—the same as crustacean shellfish, and they share a lot of similar proteins,” says Philip Johnson, an assistant professor in the food science and technology department and member of the FARRP team. “And the fact appears to be that if you are currently allergic to shellfish, you may well also react to insects.” Johnson is one of FARRP’s proteomics experts: He investigates the molecular aspects of proteins, identifying and analyzing the structure and sequence of allergens. He and Melanie Downs, an assistant professor in the food science and technology department and the other proteomics expert on the FARRP team, utilize mass spectrometry to obtain the level of detail necessary to characterize allergens and other proteins. This information aids in unraveling the mystery of why certain food proteins are allergenic and others aren’t. “While we still have limited information about what causes certain food proteins to be allergenic, we do know that these allergens fall into a relatively small number of protein families or groups,” Downs points out. There are other clues: Besides similarities in molecular structure or sequence, allergenic proteins tend to be quite abundant in foods that cause allergies and are usually resistant to digestion. “It would seem quite logical that a protein that’s difficult to digest … leaves something for the immune system to recognize.” Johnson explains. “So with food allergy, the response we see against food [allergens] is actually an immune response against parasites. It’s an [immunoglobulin E]-based response, and the body usually would use it to fight parasites.” Downs cautions that although these clues are very useful, nothing is 100% conclusive. “Understanding why some foods and some specific proteins from foods are more likely to be allergenic than others is still an area of very active research, with a number of unanswered questions,” she says.
The similarity of food proteins to known allergens is also useful in predicting whether other novel foods (i.e., foods not commonly consumed) could pose an allergy risk. For example, in some Westernized countries, insects constitute a relatively novel food source of protein powders and flours, but they share the same characteristics of a group of foods that Westerners regularly consume. “Insects are arthropods—the same as crustacean shellfish, and they share a lot of similar proteins,” says Philip Johnson, an assistant professor in the food science and technology department and member of the FARRP team. “And the fact appears to be that if you are currently allergic to shellfish, you may well also react to insects.” Johnson is one of FARRP’s proteomics experts: He investigates the molecular aspects of proteins, identifying and analyzing the structure and sequence of allergens. He and Melanie Downs, an assistant professor in the food science and technology department and the other proteomics expert on the FARRP team, utilize mass spectrometry to obtain the level of detail necessary to characterize allergens and other proteins. This information aids in unraveling the mystery of why certain food proteins are allergenic and others aren’t. “While we still have limited information about what causes certain food proteins to be allergenic, we do know that these allergens fall into a relatively small number of protein families or groups,” Downs points out. There are other clues: Besides similarities in molecular structure or sequence, allergenic proteins tend to be quite abundant in foods that cause allergies and are usually resistant to digestion. “It would seem quite logical that a protein that’s difficult to digest … leaves something for the immune system to recognize.” Johnson explains. “So with food allergy, the response we see against food [allergens] is actually an immune response against parasites. It’s an [immunoglobulin E]-based response, and the body usually would use it to fight parasites.” Downs cautions that although these clues are very useful, nothing is 100% conclusive. “Understanding why some foods and some specific proteins from foods are more likely to be allergenic than others is still an area of very active research, with a number of unanswered questions,” she says.
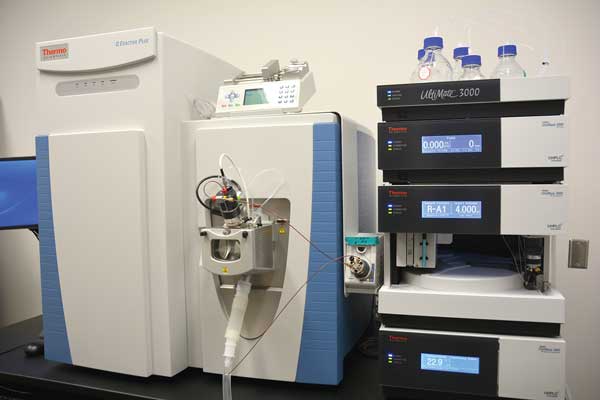
Conclusive answers to why certain foods cause allergies may be elusive, but one thing is clear: There is no cure for food allergies, so detecting food allergens is critical. FARRP pioneered methods to detect food allergens and continues to perfect them. These methods are enzyme-linked immunosorbent assay (ELISA), which uses antibodies to detect allergens; polymerase chain reaction, which determines DNA sequences; and mass spectrometry, which identifies molecules by measuring mass overcharge. Of these methods, ELISA is the most widely used. FARRP has developed 14 different ELISA tests since 1995 and has a licensing agreement with Neogen Corp. to distribute these tests commercially. FARRP also employs skilled laboratory analysts who perform allergen testing for more than 85 food companies. Prior to 1995, such immunochemical testing services were nonexistent; now food-allergen testing is a significant business around the world.
As food allergies affect more of the world’s population, the faculty, analysts, and other staff at FARRP will continue to provide the expertise, research, and services needed to make food products safe. If and when a cure for food allergies is developed, FARRP will have played a significant role in discovering it.
Food Allergens and Food Science
 Proteins cans stimulate the immune system, which is why they are the only food components that can elicit allergies. Allergenic foods are high in protein, and the proteins that induce allergic responses tend to be abundant in allergenic foods. Various food processing techniques can affect the allergenicity, or potency, of allergens in food—making allergens more or less potent, but because the allergen is still present, the food can still cause reactions. It would thus seem logical to remove allergens from foods through genetic engineering. “People have tried to do that, and what they find, in fact, is that life is more complicated than we would imagine,” says Richard Goodman, research professor, FARRP. Most allergenic foods have more than one protein that causes allergies, and not everyone with the same food allergy reacts to the same protein. For example, “there are probably 15 to 17 proteins in peanuts that have been identified as allergens,” says Steve Taylor, co-director of FARRP, so designing a food without its allergenic proteins is very difficult to do. “In theory, we can take a peanut and cut out the pieces of DNA that encode those proteins,” Goodman says, but “the major allergens make up most of the protein in the peanut. So if we remove them and don’t replace them with something else, will we have a peanut and will it be nutritious?” Likewise, the allergenic proteins in wheat, barley, and rye (the grains that contain gluten) provide properties that make it possible to make bread. Glutens and gliadins make things stick together and allow the formation and expansion of bread. Cutting out all of the gluten genes in wheat would probably render it not useful for bread-making. “You’re much better off getting other sources of grains that can make something like a bread,” Goodman says.
Proteins cans stimulate the immune system, which is why they are the only food components that can elicit allergies. Allergenic foods are high in protein, and the proteins that induce allergic responses tend to be abundant in allergenic foods. Various food processing techniques can affect the allergenicity, or potency, of allergens in food—making allergens more or less potent, but because the allergen is still present, the food can still cause reactions. It would thus seem logical to remove allergens from foods through genetic engineering. “People have tried to do that, and what they find, in fact, is that life is more complicated than we would imagine,” says Richard Goodman, research professor, FARRP. Most allergenic foods have more than one protein that causes allergies, and not everyone with the same food allergy reacts to the same protein. For example, “there are probably 15 to 17 proteins in peanuts that have been identified as allergens,” says Steve Taylor, co-director of FARRP, so designing a food without its allergenic proteins is very difficult to do. “In theory, we can take a peanut and cut out the pieces of DNA that encode those proteins,” Goodman says, but “the major allergens make up most of the protein in the peanut. So if we remove them and don’t replace them with something else, will we have a peanut and will it be nutritious?” Likewise, the allergenic proteins in wheat, barley, and rye (the grains that contain gluten) provide properties that make it possible to make bread. Glutens and gliadins make things stick together and allow the formation and expansion of bread. Cutting out all of the gluten genes in wheat would probably render it not useful for bread-making. “You’re much better off getting other sources of grains that can make something like a bread,” Goodman says.
Therefore, the best thing the food industry can do to prevent food allergies is practice prevention and vigilance. “The food industry has the responsibility to control allergen residues in their facilities,” Taylor says. “Shared facilities and shared equipment are a fact of life. You [have] to figure out how to clean it, how to have a validated allergen control program, how to prevent residues from getting into products where they don’t belong, and I think a lot of companies are controlling allergens very, very well.” Taylor’s advice on prevention extends beyond the food industry to consumers. “The other thing we need to think about is, how do we prevent young infants from being sensitized in the first place?” The LEAP (Learning Early About Peanuts) study, tested the hypothesis that regular consumption of peanut-based products, when initiated during infancy, would induce the body’s tolerance of peanuts instead of allergic reactions. At the conclusion of the study, 17% of the children who avoided peanuts developed peanut allergy by the time they were age five. Only 3% of the children who ate peanut snacks developed allergy by age five. “I think that now we have to change the advice we give to mothers about how they feed their babies,” Taylor says, referring to the advice that mothers avoid giving their children peanuts at an early age. “I think that is going to be really difficult.”
Toni Tarver is senior writer/editor of Food Technology magazine ([email protected]).
