Food Technology Magazine | Digital Exclusive
Experts to U.S. Senate: 'Food is Medicine' Boosts Health, Economy
The U.S. Senate Committee on Health, Education, Labor, and Pensions heard testimony from four experts on how “food is medicine” programs can improve national health, reduce healthcare costs, and energize local food systems.
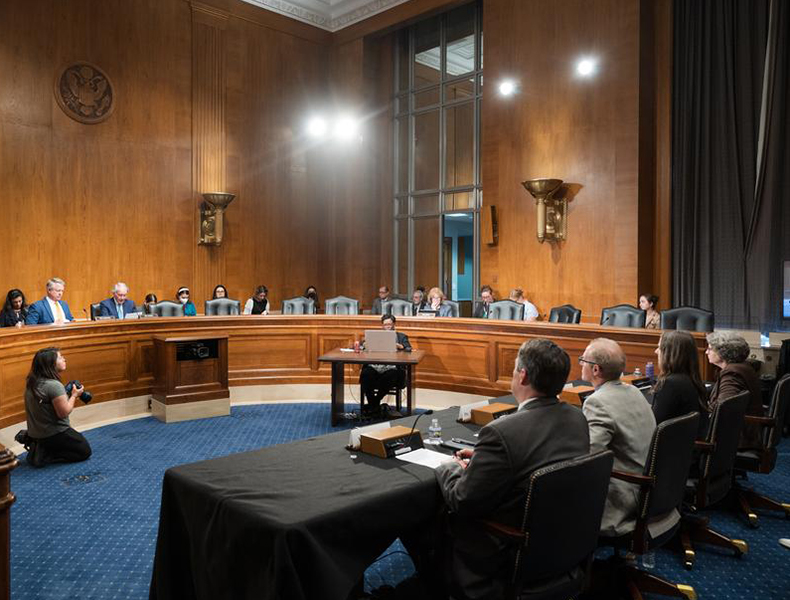
The U.S. Senate Committee on Health, Education, Labor, and Pensions hears testimony. Photo courtesy of the U.S. Senate
Food is medicine” programs, such as medically-tailored meals and produce prescriptions, have the opportunity to improve health and stimulate local economies, according to a panel of experts at the U.S. Senate Committee on Health, Education, Labor, and Pensions’ hearing on May 21, 2024.
The committee held a hearing entitled “Feeding a Healthier America: Current Efforts and Potential Opportunities for Food is Medicine.” The hearing featured witness testimony from four experts: Jean Terranova, senior director of policy and research at Community Servings in Boston; Erin Martin, founder and director of FreshRx Oklahoma in Tulsa, Okla.; Dr. Dariush Mozaffarian, director of the Food is Medicine Institute at Tufts University in Boston; and James Carter Williams, CEO and managing principal at iSelect Fund in St. Louis.
Mozaffarian explained that nutrition-related illness is becoming more prevalent throughout the United States. “Poor nutrition is the top cause of death and disability in the United States,” he explained. “I should drop the microphone right there.”
The majority of healthcare costs in the country are related to preventable diseases, which puts lower-income families at a higher risk, said Mozaffarian. He believes that “food is medicine” therapies have the unique opportunity to solve two problems at once: improve health and save money.
“There’s almost nothing in healthcare that can do both of those things,” he testified. “Food is medicine programs can support local farmers and regional food systems, serving as an economic engine for rural communities.”
Terranova described some of the outcomes of patients served through Community Servings, which was founded to address the HIV/AIDS crisis in 1990.
“Chuck, a 66-year-old with diabetes and vascular issues, has lost over 50 pounds and avoided a foot amputation since receiving a cardiac diabetic diet from Community Servings,” she said. “And Janet, a 60-year-old with an auto-immune disease and cancer, credits Community Servings with taking an intimidating burden off her plate by providing her with medically tailored meals.”
Following the experts’ testimony, members of the committee asked questions about how best to implement food is medicine programs into the healthcare system. One key aspect to consider, according to FreshRx’s Martin, is that these programs need to provide education for patients—not just access to healthy foods.
“From the studies that I’ve read and how we’ve enacted this program, I think the best results come from programs that are a hybrid model,” she said. “Delivering food has impact, but [we need to] empower people to have the knowledge to continue those behavioral changes.”
When asked by committee members about the importance of research into food is medicine initiatives, the panelists agreed that more government funding is needed to grow these programs across the country.
“I really liked the NIH [National Institutes of Health] concept of these Food is Medicine Centers of Excellence, built on the Cancer Centers of Excellence model of the 1970s,” shared Mozaffarian. “These Centers of Excellence integrate patient care with community outreach and education. I think having these hubs of knowledge generation across the country would be really important.”ft






