Mycotoxins and Their Health Impacts
FOOD SAFETY AND QUALITY
Although mycotoxins were identified as causative agents of illness in humans and animals in the last century, the illnesses they are associated with have been recognized for centuries. For instance, the French recognized “St. Anthony’s Fire” in the 11th century AD. The illness is believed to be caused by consumption of rye contaminated with ergot alkaloids produced by the fungus Claviceps purpurea (Agriopoulou et al. 2020). Interestingly, a study published in Science in 1976 debuted a hypothesis that the anomalous habits of the accused in the witchcraft trials of 1692 (Salem, Massachu-setts) were linked to ergotism caused by the ergot fungus, which can be found in rye, wheat, and other cereal grains (Caporael 1976). In the early 20th century, Shoshin-kakke, acute cardiac beriberi, was observed in Japan. The yellow-rice toxins, such as citrinin and citreoviridin, have been associated with the disease (Saito et al. 1971). In the early 1960s, the death of about 100,000 turkeys in England resulted in an investigation of the turkey “X” disease, which revealed that aflatoxin, produced by Aspergillus flavus, was present in turkey feed (peanut meal) and responsible for the illness (Blount 1961). In the 21st century, aflatoxins, produced by many species of the fungus Aspergillus, are considered inevitable contaminants in the global food supply, especially in commodities such as corn and peanuts, and their levels are regulated by various agencies. Other mycotoxins, such as deoxynivalenol, diacetoxyscirpenol, and T-2 and HT-2 toxins, affecting the world’s grain supply, are considered bioterrorism threat agents (CDC 2020).
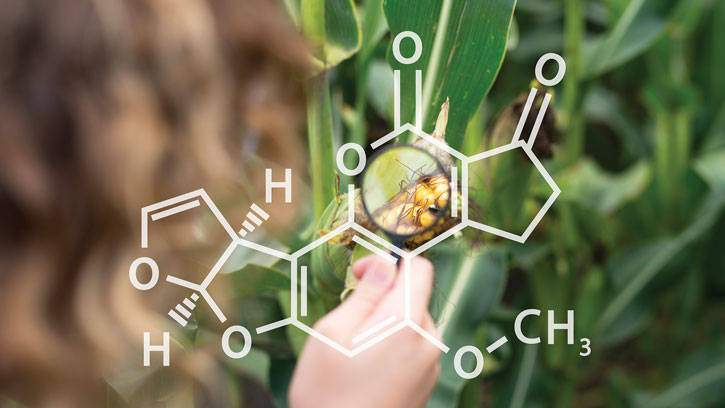
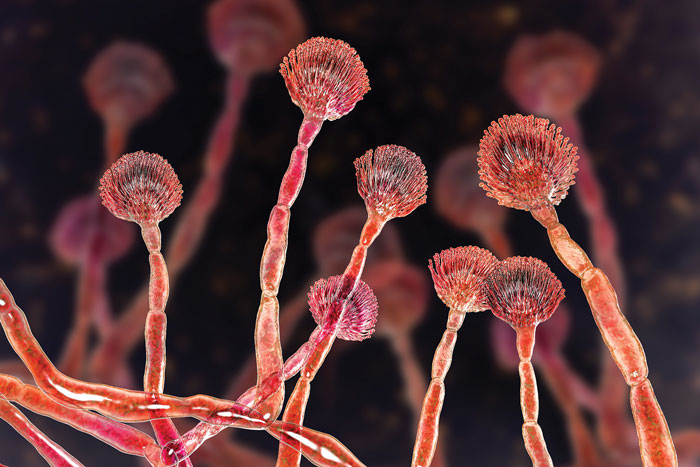
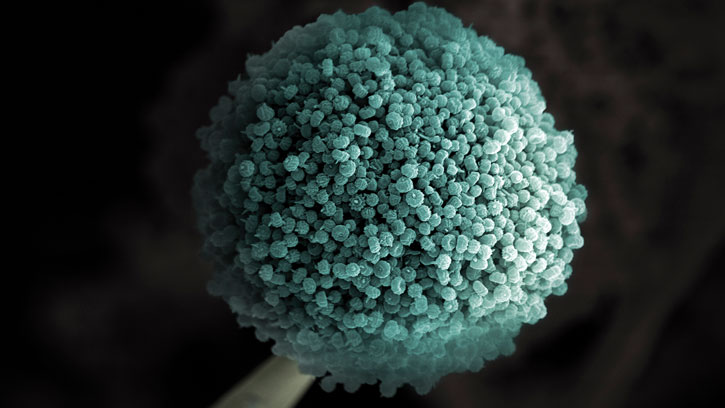
Mycotoxins are toxic secondary metabolites produced by certain fungi. Mycotoxins can readily enter the food supply chain through fungal infection of agricultural commodities in the field, during harvest, postharvest storage, or processing and transportation. The major producers of mycotoxins include certain species within three fungal genera: Aspergillus, Fusarium, and Penicillium. Fusarium species are significant for contamination of plants in the field. Aspergillus species tend to infect plants during growth in subtropical and tropical climates. Aspergillus and Penicillium species are frequently linked to contamination of agricultural commodities during postharvest storage (Agriopoulou et al. 2020).
Toxic Effects
Consumption of mycotoxin-containing food or feed may induce adverse health effects in humans or animals. With more than 100 species, Aspergillus contains several that are capable of producing mycotoxins, including aflatoxins, cyclopiazonic acid, ochratoxin A, and sterigmatocystin. Certain Aspergillus species may produce citrinine, patulin, and penicillic acid, which are also produced by Penicillium species. The Aspergillus mycotoxins of greatest implication are aflatoxins, species-specific toxins produced by A. flavus, Aspergillus parasiticus, and Aspergillus nominus, and Ochratoxin A, produced by Aspergillus ochraceus, Aspergillus carbonarius, and Aspergillus niger (Matthews et al. 2017).
Aflatoxins are considered to be the most toxic among the range of mycotoxin classes, with Aflatoxins B1, B2, G1 and G2 of principal concern. Aflatoxins M1 and M2 are produced from aflatoxins B1 and B2, respectively, in lactating animals and are consequently excreted in milk. Aflatoxins exhibit acute and chronic toxicity in humans and animals. Several outbreaks of acute aflatoxicosis have been reported in quite a few countries although acute toxicity is generally considered infrequent in humans. Vomiting, abdominal pain, jaundice, pulmonary edema, coma, convulsions, and death are among the symptoms of acute aflatoxicosis in humans. Aflatoxins are genotoxic (DNA-damaging) carcinogens. Long-standing exposure to aflatoxins has been associated with liver diseases, including cancer, cirrhosis, hepatitis, and jaundice. Research has shown a correlation between aflatoxin consumption and the incidence of primary liver cancer in Central Africa and Southeast Asia. Aflatoxins also have immunosuppressive effects (Bennett and Kich 2003), which is significant because immunosuppression can increase susceptibility to infectious diseases by hindering antibody production, primarily in individuals and populations with chronic aflatoxin ingestion. Reye’s syndrome, with symptoms of encephalopathy and visceral degeneration in children, has been linked to aflatoxin toxicity (Marin et al. 2013). Aflatoxin intake can cause serious illness in animals, especially cancer of the liver, colon, and kidneys. In cattle, poor feed conversion, low weight gain, and poor milk yields are observed with steady, low-level aflatoxin intake (Richard 2007). Ochratoxin A produced by A. ochraceus has immunosuppressant, immunotoxic, genotoxic, neurotoxic, teratogenic (reproductive) and carcinogenic effects. Research indicates a strong correlation between nephropathy (kidney disease) and ochratoxin A exposure in humans and animals (Agriopoulou et al. 2020).
Among the Penicillium species, more than 80 are documented toxin producers. The most important toxins include ochratoxin A, citrinin, patulin, cyclopiazonic acid, citreoviridin, penitrem A, roquefortine, and secalonic acids. The Penicillium mycotoxins that affect liver or kidney function, by acute or chronic exposure, are usually asymptomatic in humans or animals. Those that affect nervous system function (i.e., neurotoxins) are characterized by continuous trembling in animals. Ochratoxin A, which is lipid-soluble, is not excreted efficiently and can accumulate in meat animals that consume contaminated feed and subsequently cause exposure in humans consuming the meat (Matthews et al. 2017). Ochratoxin A has been implied to cause an illness called “Balkan endemic neuropathy,” a kidney disease with high mortality in Eastern Europeans living near tributaries of the Danube River (Pfohl-Leszkowicz and Manderville 2007).
Citrinin is a significant renal toxin in all animal species tested, causing kidney degeneration with symptoms including watery diarrhea, higher water consumption, and weight loss. Assessing citrinin’s significance for human health has been challenging (Bennett and Kich 2003). Patulin causes neurotoxic, immunotoxic, carcinogenic, teratogenic (birth defects), and mutagenic effects in cell cultures. Immunotoxic and neurotoxic effects are observed in animals; however, patulin does not appear to exhibit chronic toxicity in humans (Bennett and Kich 2003). Citreoviridin is a neurotoxin in humans and animals, resulting in heart distress, difficulty breathing, nausea/vomiting, psychological symptoms (pain, suffering, and agitation), paralysis, and muscular atrophy (Bennett and Kich 2003).
Fusarium species produce several toxic or biologically active metabolites, called trichothecenes, which at high concentrations cause acute symptoms such as allergic reactions, vomiting, and diarrhea in humans. Trichothecenes are also associated with reduced weight gain and immune dysfunction in animals (Wu et al. 2014). Zearalenone, the toxicity of which in humans is not fully understood, causes uterotrophic (anti-reproductive) effects in animals such as pigs (Agriopoulou et al. 2020). Fumonisins may have neurotoxic effects in some animals. Fusarium verticillioides has been associated with human esophageal cancer (Bennett and Klich 2003).
There are several challenges to assessing the human toxicity of mycotoxins. Level and duration of exposure is one; another is the difficulty of assessing immuno-suppressant effects in immunocompromised populations. Further, a particular mycotoxin may modulate the toxicity of another mycotoxin occurring in foods, yet another layer of challenge in accurate evaluation of mycotoxicity.
Mycotoxin Exposure
While human exposure to mycotoxins is usually through consumption of plant foods, exposure through consumption of foods of animal origin such as dairy and meat products may also occur as a result of mycotoxin contamination of animal feed. Aflatoxins are extremely common in stored agricultural commodities and occur more frequently in commodities originating from the tropical and subtropical climates, including grains (corn, others), nuts (pistachio nuts, peanuts, Brazil nuts, others), dried fruit (apricots, figs, and others), and food products derived from these commodities. The diversity of these agricultural commodities indicates a significant potential for human exposure to aflatoxins.
Various food processing technologies modify mycotoxin levels in processed commodities. The effect of food processing on complete removal, decrease, or increase of mycotoxin levels appears to be a mycotoxin-dependent phenomenon. Examples of mycotoxin reduction through food processing include cleaning and sorting/grading of cereal grains and fruits, producing flour through milling of various cereal grains, and thermal processing in various forms. Food processing that involves germination of cereals (malting barley for brewing) may increase mycotoxin level in germinated cereals (Park et al. 1999).
Mycotoxins levels are regulated by the U.S. Food and Drug Administration (FDA 2020). The European Food Safety Authority collects and evaluates mycotoxin occurrence data and provides scientific advice for risk managers to use in setting maximum levels in food and feed (EFSA 2020). Through the work of its Committee on Contaminants in Food, the Codex Alimentarius Commission develops standards, guidelines, and codes of practice relating to contaminants, including limits for mycotoxins (FAO and WHO 2018).
A ‘Renewed View’ Needed
Consumer demand for plant-based foods and interest in animal-based foods originating from animals fed plant-based feed has been on the rise. Thorough understanding of mycotoxins occurring in the plant-based food supply is critical, and a better understanding of mycotoxins occurring in animal feed is needed.
In recent years, certain mycotoxins have appeared in atypical agricultural commodities and associated food products and/or unusual regions/climates. Global warming is likely to play a role in this (Medina et al. 2015). The significance of having a “renewed” overview of the well-documented mycotoxins now occurring in atypical commodities, regions, and climates cannot be overemphasized.
New research leads to newly discovered mycotoxins. Study of the occurrence and toxicological effects of these mycotoxins is critical.
Maximum and guidance limits for mycotoxins in specific food and feed products have been established to aid development of effective risk management measures and ensure safety of human food and animal feed. Differences in mycotoxin action levels exist among countries, regions, and entities. Fair international trade requires further harmonization.
REFERENCES
Agriopoulou, S., E. Stamatelopoulou, T. Varzakas. 2020. “Advances in Occurrence, Importance, and Mycotoxin Control Strategies: Prevention and Detoxification in Foods.” Foods 9: 137. doi:10.3390/foods9020137.
Bennett, J. W., M. Klich. 2003. “Mycotoxins.” Clin. Microbiol. Rev. 16(3): 497–516.
Blount, W. P. 1961. Turkey “X” Disease. Turkeys 9: 52, 55–58, 61, 77.
Caporael, L. 1976. “Ergotism: The Satan Loosed in Salem?” Science 192: 21–26. doi:10.1126/science.769159.
CDC. 2020. “Toxins.” Centers for Disease Control and Prevention. https://www.cdc.gov/biomonitoring/toxins.html.
EFSA. 2020. “Mycotoxins.” European Food Safety Authority. https://www.efsa.europa.eu/en/topics/topic/mycotoxins.
FAO and WHO. 2018. “Codex Alimentarius: Understanding Codex.” 5th ed. Food and Agriculture Organization of the United Nations and World Health Organization. Rome.
FDA. 2020. “Natural Toxins and Mycotoxins.” U.S. Food and Drug Administration. https://www.fda.gov/food/chemicals-metals-pesticides-food/natural-toxins-and-mycotoxins.
Marin, S., A. J. Ramos, G. Cano-Sancho, V. Sanchis. 2013. “Mycotoxins: Occurrence, Toxicology, and Exposure Assessment.” Food Chem. Toxicol. 60: 218–237. doi: j.fct.2013.07.047.
Matthews, K. R., K. E. Kniel, T. J. Montville. 2017. “Food Microbiology: An Introduction.” Washington, DC: ASM Press.
Medina, A., A. Rodríguez, N. Magan. 2015. “Climate Change and Mycotoxigenic Fungi: Impacts on Mycotoxin Production.” Curr. Opin. Food Sci. 5: 99–104. doi.org/10.1016/j.cofs.2015.11.002.
Park, D. L., H. Njapau, E. Boutrif. 1999. “Minimizing Risks Posed by Mycotoxins Utilizing the HACCP Concept.” Food Nutr. Agric. 23: 49–54. http://www.fao.org/3/x2100t/X2100t08.htm.
Pfohl-Leszkowicz, A., R. A. Manderville. 2007. “Ochratoxin A: An overview on Toxicity and Carcinogenicity in Animals and Humans. Mol. Nutr. Food Res. doi:10.1002/mnfr.200600137.
Richard, J. L. 2007. “Some Major Mycotoxins and Their Mycotoxicoses: An Overview.” Int. J. Food Microbiol. 119(1–2): 3–10. doi: j.ijfoodmicro.2007.07.019.
Saito, M., M. Enomoto, T. Tatsuno. 1971. Yellowed Rice Toxins Luteoskyrin and Related Compounds, Chlorine-Containing Compounds, and Citrinin. In Microbial Toxins, Vol. 6: Fungal Toxins, edited by A. Ciegler, S. Kadis, S. J. Ajl. New York: Academic Press.
Wu, F., J. D. Groopman, J. J. Pestka. 2014. “Public Health Impacts of Foodborne Mycotoxins.” Annu. Rev. Food Sci. Technol. 5(1): 351–372. doi:10.1146/annurev-food-030713-092431.