COVID-19, Wet Markets, and Food Safety
FOOD SAFETY AND QUALITY
Given the impact of COVID-19, we are being re-educated and updated on safe practices in the workplace, social settings, shopping, and daily life. Quarantines and physical distancing have become imperative. Although the need to obtain food continues, grocery stores, farmers markets, and roadside stands have all been affected. COVID-19 is not known to be transmitted by food or its packaging (Seymour 2020), yet the public is concerned about proper food handling.
Wet vs. Wild Markets
“Wet markets,” which get their name from the presence of liquid—such as tanks of water containing live fish and melting ice used to keep meat cold—are a staple in Asia but are found worldwide including in the United States. Like farmers markets, wet markets typically have open-air stalls selling produce, fresh meats, and seafood. Live animals such as poultry, fish, and shellfish may also be slaughtered and sold on-site (Maron 2020). Wet markets become “wild markets” when live wild game animals are present. The now infamous Huanan Seafood Wholesale Market in Wuhan, China, had a wild animal section where snakes, beavers, porcupines, baby crocodiles, and other species were slaughtered on-site prior to sale (Maron 2020). The market is believed by many to be ground zero for COVID-19 and zoonotic transfer from bats into the human population. However, a World Health Organization food and animal disease expert stated that it was not clear whether the virus came from an infected live animal or a human vendor or shopper (Anonymous 2020a).
While wet markets do exist in the United States, no uninspected, wild game meat may be sold due to state and federal regulations. Commercially raised game or harvested meats may be sold but must pass through a U.S. Department of Agriculture- or state-inspected processing facility. These nonamenable wild species have the same inspection and regulation requirements as traditionally farmed species such as beef and poultry. For more information on the processing and regulation of game meats in the United States, see the article “Safe Consumption of Wild Game” in the March 2020 issue of Food Technology.
Exotic Food Myths, Risky Behaviors
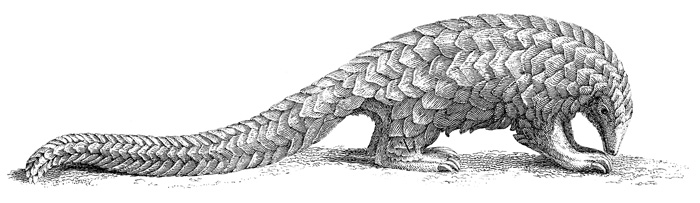
In some cultures, there are beliefs that meat or other products from certain wild animals provide therapeutic effects (Li et al. 2020). For example, meat from a pangolin, a scale-covered mammal, is believed to reduce rheumatism and its bile is believed to improve eyesight (Li et al. 2020). Pangolins are one of the most trafficked mammals in Asia and increasingly, Africa; their meat is considered a delicacy and their scales are used in traditional medicine and folk remedies (Anonymous 2020b). Pangolins are thought to possibly be the intermediate host for transmission of the coronavirus from bats to humans. This is based on comparisons of the amino acid compositions of the spike proteins on viral surfaces (Zhang et al. 2020).
Eating bush meat is risky. A contemporary trend, more travelers are seeking exotic cuisine on international excursions. Some in pursuit of new gastronomic experiences consume and encounter wildlife in wild markets. Unfortunately, this may pose health risks due to zoonotic transmission of severe acute respiratory syndrome (SARS), H1N1 influenza, bird flu, and novel coronavirus pneumonia (Ying et al. 2020). A behavior called “the mukbang” involves people eating in front of internet audiences strange or dangerous food. In 2016, one broadcast featured someone eating bat soup. Sometimes the animals are eaten raw or live (Li et al. 2020). According to a survey conducted in southeast Asia and commissioned by the World Wildlife Fund, 93% of the participants supported government closure of unregulated wildlife markets (Maron 2020).
Foodborne Viruses
Viruses causing human foodborne illness cannot grow in foods. Viruses found on foods are the result of fecal contamination or handling by infected persons (Seymour and Appleton 2001). Viral foodborne pathogens are those that can infect a person via the gastrointestinal (GI) tract due to their acid resistance. The most common causes of viral GI distress are norovirus and hepatitis A (Seymour and Appleton 2001). Data collected from 2004 to 2012 showed that most produce-related outbreaks in the United States and European Union were caused by norovirus followed by Salmonella bacterial species (Callejon et al. 2015). Both viral and bacterial outbreaks have been closely tied to the consumption of raw produce consumed in salads; and in the European Union, norovirus on berries was cited as the major culprit in viral outbreaks (Callejon et al. 2015).
These viruses are difficult to culture in the lab; therefore, most research uses viral surrogates such as feline calicivirus or murine (mouse) norovirus, which can be grown in cell cultures (Richards 2012). Unlike enteric viruses, respiratory viruses such as the coronavirus have not been shown to be spread by eating contaminated food (Seymour and Appleton 2001, Seymour et al. 2020). In a recent interview, Lee-Ann Jaykus, William Neal Reynolds Distinguished Professor of Food Science at North Carolina State University, said: “If the [COVID-19] virus were present in a food, it would still not be likely to infect the person eating that food–although it’s probably not impossible. However, for such an infection to occur, all the right factors would need to be in place. I believe putting our attention on foods takes attention away from what we already know works, which is social distancing and isolation” (Shipman 2020).
Coronaviruses and Food
What do we know about coronaviruses and food or food contact surfaces? Not much. Early research indicated that some coronaviruses are not acid tolerant. A study with human coronavirus 229E found that virus infectivity was at a maximum at pH 6.0 when incubated in cell cultures at either 4ºC or 33ºC (Lamarre and Talbot 1989). At 33ºC, infectious titers dropped precipitously from 5.0 log10 plaque forming units (PFU)/mL to below detection levels (<1.3 log10 PFU/mL) when the pH decreased from 4.5 to 4.0 (Lamarre and Talbot 1989).
The pH of gastric juice in the human stomach lumen is between 1.5 and 3.5 (Wikipedia 2020). While human coronavirus strain 229E would probably not survive passage through the upper digestive tract via consumption of contaminated food, recent studies with COVID-19 question whether it targets the human GI tract through binding of angiotensin-converting enzyme 2 expressed by epithelial cells in the small intestine (Liang et al. 2020). Studies with the coronavirus strain MERS-CoV suggested that the human GI tract may be an alternative infection route (Zhou et al. 2017). In the MERS-CoV study, intragastric inoculation of MERS-CoV (105 PFU) caused a lethal infection in human dipeptidyl peptidase 4 transgenic mice. As the enteric infection progressed, live virus emerged in the lung tissue indicative of a secondary respiratory infection. Liang et al. (2020) cautioned that human intestinal cells might be vulnerable to attack by COVID-19 and that the incidence of diarrhea should receive more attention by clinicians.
The National Institutes of Health cited a study revealing that COVID-19 was infectious in aerosols for up to three hours and on plastic and stainless steel surfaces for up to three days (NIH 2020). Although these results suggest that humans can be infected by breathing aerosols or touching contaminated surfaces, these infections were induced in laboratory cell cultures.
Furthermore, the interaction of COVID-19 contamination of food contact surfaces and subsequent transfer of infectious particles to foods has not been explored. And infectivity rates in humans need evaluation. Good food safety practices—including rinsing produce with clean water prior to
eating and cooking meats to recommended internal temperatures—continue to be important. Produce should not be washed with dish soap and detergents or treated with disinfectants not intended for produce (Seymour et al. 2020).
Nutraceuticals and COVID-19
Food bioactive compounds were studied to see if they provided any inhibitory effects on COVID-19 proteases or polymerases. In silico modeling evaluating binding energies between compounds and viral proteins found that several candidates (phycocyanobilin, riboflavin, cyanidin, daidzein, and genistein) derived from fruits, vegetables, whole grains, and legumes have the potential to be potent inhibitory compounds (Pendyala and Patras 2020). The authors said further in vitro and in vivo research is needed to validate their preliminary results.
Other researchers are looking at coconut oil as a treatment. Monolaurin and lauric acid have antiviral activities, being able to destroy the membrane of lipid-coated viruses. As reported in a recent IFTNEXT newsletter item, because coconut oil contains high levels of lauric acid, it is being considered as a nutraceutical therapy.
What’s Next?
By the time this article goes to publication, we will undoubtedly know considerably more about COVID-19 and the causative virus (SARS-CoV-2). Less dangerous surrogates should be identified to increase the pace of research and lower the risk to scientists working with the coronavirus. Attitudes concerning risky consumption behaviors will need to evolve. Experts and respected authorities need to bust myths about wild game therapeutics. Social media should address opinions about what is trendy or outrageous to eat. All risky food consumption behaviors should be discouraged by peers and professionals. Governments should more closely regulate wet markets and unregulated wildlife markets should be banned worldwide. Let’s use this pandemic as a call to action to reinforce proven food safety practices, provide widespread consumer education, and assist all retail outlets with science-based preventive measures.
The author thanks Ben Chapman, food safety extension specialist at North Carolina State University, for his helpful edits and suggestions.
REFERENCES
Anonymous. 2020a. “WHO Expert Believes Wuhan Wet Market Played Role in COVID Outbreak.” VOA News, May 8. https://www.voanews.com/covid-19-pandemic/who-expert-believes-wuhan-wet-market-played-role-covid-outbreak.
Anonymous. 2020b. “What Is a Pangolin?” World Wildlife Fund. https://www.worldwildlife.org/stories/what-is-a-pangolin.
Callejon, R. M., M. I. Rodriguez-Naranjo, C. Ubeda, et al. 2015. “Reported foodborne outbreaks due to fresh produce in the United States and European Union: trends and causes.” Foodborne Pathog. Dis. 12: 32–38.
Lamarre, A. and P. J. Talbot. 1989. “Effect of pH and temperature on the infectivity of human coronavirus 229E.” Can. J. Microbiol. 35: 972–974.
Li, J., J. Li, X. Xie, et al. 2020. “Game consumption and the 2019 novel coronavirus.” The Lancet 20: 275–276. doi.org/10.1016/S1473-3099(20)30063-3.
Liang, W., Z. Feng, S. Rao, et al. 2020. “Diarrhea may be Underestimated: a Missing Link in the 2019 Novel Coronavirus.” medRxiv doi:10.1101/2020.02.03.20020289. Preprint.
Maron, D. F. 2020. “‘Wet Markets’ Likely Launched the Coronavirus. Here’s What you Need to Know.” National Geographic, April 15. https://www.nationalgeographic.com/animals/2020/04/coronavirus-linked-to-chinese-wet-markets/.
NIH Research Matters. 2020. “Study Suggests New Coronavirus may Remain on Surfaces for Days.” March 11. https://www.nih.gov/news-events/nih-research-matters/study-suggests-new-coronavirus-may-remain-surfaces-days.
Pendyala, B. and A. Patras. 2020. “In Silico Screening of Food Bioactive Compounds to Predict Potential Inhibitors of COVID-19 Main Protease (Mpro) and RNA-Dependent RNA Polymerase (RdRp). ChemRxiv. doi.org/10.26434/chemrxiv.12051927.v2. Preprint.
Richards, G. P. 2012. “Critical review of norovirus surrogates in food safety research: rationale for considering volunteer studies.” Food Environ. Virol. 4: 6–13. doi:10.1007/s12560-011-9072-7.
Seymour, I. F. and H. Appleton. 2001. “A review: foodborne viruses and fresh produce.” J. Appl. Microbiol. 91: 759–773.
Seymour, N., M. Yavelak, C. Christian, et al. 2020. “Is Coronavirus a Concern on Fresh Produce?” EDIS 2020 (March). https://journals.flvc.org/edis/article/view/121334.
Shipman, M. 2020. “What we Know and Don’t Know About Food Safety and COVID-19.” April 8. https://news.ncsu.edu/2020/04/food-safety-COVID-q-and-a/.
Wikipedia. 2020. “Gastric Acid.” https://en.wikipedia.org/wiki/Gastric_acid.
Ying, T., K. Wang, X. Liu, et al. 2020. “Rethinking Game Consumption in Tourism: A Case of the 2019 Novel Coronavirus Pneumonia Outbreak in China.” Tourism Recreation Research. doi:10.1080/02508281.2020.1743048.
Zhang, Y., C. Zhang, W. Zheng, et al. 2020. “More Evidence Suggests Pangolins may Have Passed Coronavirus From Bats to Humans.” Sci. Alert, April 11. https://www.sciencealert.com/more-evidence-suggests-pangolins-may-have-passed-coronavirus-from-bats-to-humans.
Zhou, J., C. Li, G. Zhao, et al. 2017. “Human intestinal tract serves as an alternative infection route for Middle East respiratory syndrome coronavirus”. Sci. Adv. 3 (11): eaao4966. doi:10.1126/sciadv.aao4966.