Building Better Bones
NUTRACEUTICALS & FUNCTIONAL FOODS
Low bone mass and osteoporosis are two of the ill effects of poor bone health. According to the National Osteoporosis Foundation (NOF, 2002), these two conditions are a major public health threat for 55% of the people aged 50 and older in the United States-almost 44 million women and men.
Low bone mass is the most accurate predictor of fracture risk. The association between low bone mass and fracture is stronger than that between systolic blood pressure and stroke and that between serum cholesterol and coronary events (Kanis, 1994). On average, bone mass peaks at about age 30-35 and declines steadily thereafter. Adults age 30-45 years lose 1-2% of their bone mass each year. In addition, women are at four times greater risk than men of developing low bone mass.
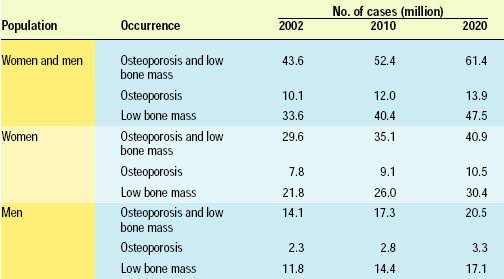 Osteoporosis is a disease of the bone characterized by low bone mass and decreased bone density. This deterioration of bone tissue can lead to bone fragility and increased susceptibility to fracture, especially of the hip, spine, and wrist. An estimated 10 million people currently have osteoporosis, approximately 80% of them women. If additional efforts are not made to prevent osteoporosis, the number affected will rise to 12 million by 2010 and 14 million by 2020 (Table 1).
Osteoporosis is a disease of the bone characterized by low bone mass and decreased bone density. This deterioration of bone tissue can lead to bone fragility and increased susceptibility to fracture, especially of the hip, spine, and wrist. An estimated 10 million people currently have osteoporosis, approximately 80% of them women. If additional efforts are not made to prevent osteoporosis, the number affected will rise to 12 million by 2010 and 14 million by 2020 (Table 1).
To increase public awareness of osteoporosis and prevention, World Osteoporosis Day, sponsored by the International Osteoporosis Foundation, took place on October 20, 2002. Its message was, “”invest in your bones: Prevent the first fracture". Preventing the first fracture is key because the risk of a "cascade" effect resulting in future fractures is high. For example, one out of five women suffering a first vertebral fracture will fracture again within one year. In addition, according to NOF, the current estimated annual price tag for America in direct medical costs for treating fractures resulting from osteoporosis is $17 billion.
Building Blocks for Strong Bones
The key to preventing osteoporosis and low bone mass is to build strong bones, especially by the age of 35. In addition to regular exercise, no smoking, and limited alcohol intake, nutrition plays an important role. Here is a closer look at some of the nutrients that serve as building blocks for healthy bones.
• Calcium is an essential nutrient for bone health. During childhood, it is required for continued bone growth, and later in life it is required for the ongoing process of bone remodeling. Calcium and other nutrients are very important for not only bone health but also dental health. Bones and teeth contain about 99% calcium.
"The body normally absorbs 25-75% of the dietary calcium we consume," said dietitian Cindy Moore, spokesperson for the American Dietetic Association and Director of Nutrition Therapy at the Cleveland Clinic Foundation, Ohio. "This is a pretty wide variation. The factors that affect this absorption rate include our age, the presence of adequate vitamin D, the body's need for calcium, and our calcium intake."
The adequate intake for calcium is 1,300 mg/day for persons age 9-18, 1,000 mg/day for those age 19b-50, and 1,200 mg/day for those 51 and older, said Moore. "Unfortunately, consumers are not getting enough calcium. Studies done between 1977 and 1978 found that the average calcium intake was 743 mg/day. This increased to 813 mg in 1995. A number of studies compiled by the National Institutes of Health indicated that young women age 12-19 average less than 900 mg/day of calcium."
A calcium deficiency is not only detrimental for bones, but can also lead to an increased risk for acquiring hypertension, colon or breast cancer, and for developing kidney stones, added Moore.
--- PAGE BREAK ---
Acknowledging that calcium deficiency is a problem in the U.S., the Suntory Water Group, Atlanta, Ga., a U.S.-based division of the Japanese group Suntory, launched a calcium-enriched water under the Hinckley Springs, Crystal Springs, and Kentwood Springs brands earlier this year. The company said the decision to produce Calcium Water had been made after the U.S. Dept. of Health, Education, And Welfare highlighted calcium deficiency as a major problem in the U.S. Drinking 2 L of the purified water per day provides 24% of the reference daily intake for calcium (1,000 mg).
Flavored milk may also be an ideal vehicle to prevent calcium deficiencies in children. Research at the University of Vermont studied the beverage patterns of nearly 4,000 children and adolescents in the U.S. They found that those who drank flavored milk had a higher total milk intake and a lower soft drink and juice drink intake than children who did not consume flavored milk. Drinking flavored milk helped increase their calcium consumption, but it did not increase overall added sugar or fat intake (Johnson et al., 2002).
•Vitamin D aids in the body's absorption of calcium, helping to form and maintain strong bones. "For individuals between the ages of 19 and 51, the daily adequate intake is 5 μg,” said Moore. "This increases to 10 μg for ages 51-70, and 15 ug for those over 70." The primary sources for vitamin D are salmon, sardines, milk, fortified ready-to-eat cereals, and cod liver oil.
Two studies presented at the International Osteoporosis Foundation's World Congress on Osteoporosis in May 2002 in Portugal (www.iofcongress.org) high-lighted the importance of vitamin D. In the first study, Marjo Lehtonen-Veromaa and colleagues at Turku University Central Hospital, Turku, Finland, looked at the importance of vitamin D and peak bone mass in adolescents. Their three year study assessed the association between vitamin D status and attainment of B peak bone mass among 171 healthy Finnish girls age 9-15 years old. Bone mineral density was assessed at the lumbar spine and femoral neck, and dietary intake of vitamin D and calcium was estimated on the basis of food-frequency questionnaires. The investigators concluded that dietary enrichment or supplementation with vitamin D warrants serious consideration to ensure adequate vitamin D status among all adolescents.
In the second study, Pierre J. Meunier of the Dept. of Rheumatology and Bone Diseases at Edouard Herriot Hospital, Lyon, France, suggested that calcium and vitamin D supplementation is equally important in older subjects in terms of preventing hip fractures. The study involved 3,270 institutionalized elderly women in Belgium, France, Germany, the Netherlands, Spain, Sweden, and the United Kingdom and assessed the cost-effectiveness of daily supplementation with 1,200 mg of elemental calcium plus 800 IU of vitamin D-3, compared to a placebo, in terms of reducing the incidence of hip fracture.
After 36 months of followup, the intent-to-treat analysis demonstrated a 25% reduction in the incidence of hip fractures among women receiving calcium and vitamin D, compared to those administered a placebo. According to Meunier, prevention strategies should be developed, at no increased cost, but with substantial cost savings over the long term. "Treating 1,000 institutionalized women with calcium-vitamin D3 continued supplementation can allow to avoid 46 fractures over a 36-month treatment period," he said.
• Phosphorus is an essential component of adenosine triphosphate (ATP). It is also a key component of DNA and RNA. Sources of phosphorus include chicken, beef, some dairy products, and lentils. Bones store about 85% of the body's supply of phosphorus, said Moore.
Research conducted at Creighton University, Omaha, Neb., indicated that osteoporosis patients should receive their calcium in the form of calcium phosphate to reduce the risk of phosphorus deficiency. Heaney and Nordin (2002) evaluated the calcium and phosphorus balance data obtained in two data sets: the first, 543 studies of healthy women aged 35-65, and the second, 93 men and women aged 19-78. "As calcium intake increases without a corresponding increase in phosphorus intake, phosphorus absorption falls and the risk of phosphorus insufficiency rises. Intakes with high calcium:phosphorus ratios can occur with use of supplements or food fortificants consisting of non-phosphate calcium salts," the researchers said. "Older patients with osteoporosis treated with current generation bone active agents should receive at least some of their calcium co-therapy in the form of a calcium phosphate preparation," they concluded.
--- PAGE BREAK ---
• Potassium found in foods such as bananas, tomatoes, and orange juice could help fight osteoporosis in postmenopausal women by helping to reduce the level of calcium losses, reported researchers from the University of California, SanB Francisco (Sellmeyer et al., 2002). The researchers, led by Deborah Sellmeyer, Assistant Adjunct Professor of Endocrinology and Metabolism, examined the effect of increased dietary sodium chloride on urine calcium excretion and bone turn-over markers in postmenopausal women and whether potassium citrate attenuates the effects of increased dietary salt.
Sellmeyer said that while there was also substantial evidence to show that dietary calcium and vitamin D can help preserve bone density, the study was the first to examine the role of potassium in preventing bone density loss exacerbated by a high-salt diet. In the study, 60 healthy postmenopausal women were placed onB a low-salt diet (2 g/day) for an initial three weeks while their level of excreted calcium was measured. The level of excreted NTX, a bone protein, was also measured. A higher NTX level indicates that more bone is being broken down, or reabsorbed, leaving women at increased risk for fractures.
At the end of three weeks, all the participants were placed on a high-salt diet (9 g/day). Half were given a potassium citrate supplement and the other half a placebo. For four more weeks, they continued the high-salt diet. At the study's end, researchers were able to compare each woman's low- and high-salt diet results individually. They were also able to compare the loss of calcium and NTX between the placebo group and the group receiving potassium.
Calcium loss increased 33% among women taking the placebo, but decreased 4% in the potassium citrate group. NTX excretion increased 23% among women taking the placebo, but increased only 7.5% in women taking potassium citrate, suggesting that their bones were remaining healthier than the bones of women receiving only the placebo.
"When they went from a low salt diet to a high salt diet plus potassium, there was no change," said Sellmeyer. But increased dietary salt led to higher levels of urinary calcium excretion in the women who received only the placebo, and their enhanced calcium excretion was associated also with increases in NTX, suggesting skeletal effects, the authors said. The potassium dosage used in the test was 3.5 g/day, about the amount in 10 bananas.
Other Nutrients Play a Role
Other nutrients also play important roles in bone health but are not discussed as much, added Moore.
• Fluoride. Most (99%) of fluoride is found in bones and teeth. It promotes deposition of calcium and phosphate in the bones. Water is the primary dietary source for fluoride.
• Manganese. Primarily located in the bone, liver, pancreas, and brain, manganese activates enzymes involved in the formation of cartilage in the bone. Dietary sources include nuts, greens, whole-wheat items, oats, tea, and some fruits.
• Magnesium. Bones serve as a reservoir for holding magnesium. It is involved with enzyme-mediated reactions such as protein synthesis. Magnesium is essential for the production of ATP. Dietary sources include cheeses, nuts, beans, and fish.
• Vitamin A. A lack of vitamin A causes bones to weaken. It is believed that this may be due to the disruption of the bone-remodeling process and failure of immature bone cells to develop properly. Dietary sources for vitamin A include beets, chicken liver, sweet potatoes, cantaloupe, and spinach.
• Vitamin K. Assisting in bone formation, vitamin K helps facilitate the process needed to allow osteocalcin, a calcium-binding protein, to strengthen the skeleton. A lack of vitamin K puts one at greater risk for bone fracture. Dietary sources include green vegetables, beets, chicken liver, and strawberries.
--- PAGE BREAK ---
Soy and Green Tea May Play a Role
There has been some discussion about soy and green tea aiding in bone health, but more research needs to be conducted before there is a final consensus. According to soy.com, Silicon Valley, Calif., Asian and vegetarian women have a lower incidence of osteoporosis than Western meat-eating women who have similar or lower calcium intakes. The Asian and vegetarian women typically consume more soy foods than Western women, and therefore soy may be contributing to the reduced risk for bone disease.
Soy indirectly influences calcium levels by enhancing the amount of calcium retained in bone. It appears that both the protein and isoflavones in soy contribute to this beneficial effect. It is thought that the soy isoflavone daidzein is similar to a drug used in Asia and Europe to treat osteoporosis.
Information from the United Soybean Board (www.talksoy.com) stated that isoflavones found in soy protein may also play an important role in protecting bones. A study at the University of Illinois at Urbana concluded that consuming soybean isoflavones can increase bone mineral content and bone density. As little as 40 g of soy protein consumed each day for six months led to positive results in a test group of postmenopausal women.
Tea may play a similar role in strengthening the bones. Researchers have hypothesized that bone mineral density may be influenced by chemical compounds such as the phytoestrogens and fluoride contained in tea extracts. Both may enhance bone strength, said researchers at National Cheng Kung University Hospital in Tainan, Taiwan. The bone-strengthening benefits of tea occurred in people who drank an average of nearly two cups daily of black, green, or oolong tea for at least six years. The study (Wu et al., 2002) was based on surveys of 1,037 men and women age 30 and older who were questioned about tea-drinking habits and took bone mineral density tests. The researchers accounted for other factors affecting bone strength, including gender, age, body-mass index, and lifestyle.
Habitual tea consumption, especially for more than 10 years, had significant beneficial effects on bone mineral density of the total body, lumbar spine, and hip regions in adults. Habitual drinkers for 6-10 years had a hip-bone density 2.3% higher than that in nonhabitual tea drinkers, said coauthor Chih-Hsing Wu. Similar results were found regardless of type of tea consumed.
Diet and Exercise Important
In addition to consuming the right nutrients, it is also important that consumers think about things they might or might not be doing, reminded Moore. "Diets high in sodium can increase calcium excretion and increase the risk for osteoporosis. In addition, some other types of food components may reduce calcium absorption and increase calcium excretion. These include phytates, oxalates, and caffeine. Regular weight-bearing exercise, on the other hand, can actually enhance bone remodeling and prevent loss of bone mass."
by LINDA MILO OHR
Contrtibuting Editor
Chicago, Ill.
References
Heaney, R.P. and Nordin, B.E. 2002. Calcium effects on phosphorus absorption: Implications for the prevention and co-therapy of osteoporosis. J. Am. College Nutr. 21: 239-44.
Johnson, R.K., Frary, C., and Wang, M.Q. 2002. The nutritional consequences of flavored-milk consumption by school-aged children and adolescents in the United States. J. Am. Dietetic Assn. 102: 853-856.
Kanis, J.A. 1994. Osteoporosis and its consequences. Chpt. 1 in “Osteoporosis,” pp. 1-20. Blackwell Science Inc., Cambridge, Mass.
NOF. 2002. America’s bone health: The state of osteoporosis and low bone mass in our nation. Natl. Osteoporosis Foundation, Washington, D.C. (www.nof.org).
Sellmeyer, D.E., Schloetter, M., and Sebastian, A. 2002. Potassium citrate prevents increased urine calcium excretion and bone resorption induced by a high sodium chloride diet. J. Clin. Endocrinol. Metab. 87: 2008-2012.
Wu, C.H., Yang, Y.C., Yao, W.J., Lu, F.H., Wu, J.S., and Chang, C.J. 2002. Epidemiological evidence of increased bone mineral density in habitual tea drinkers. Arch. Intern. Med. 162: 1001-6.


